Researchers at PUMCH have achieved a significant advancement in precision cervical cancer treatment, developing an AI-powered system that improves how doctors make radiotherapy decisions. The team, led by Zhang Fuquan, Director of Department of Physical Medicine & Rehabilitation, and Hu Ke, Director of Department of Radiotherapy, created an innovative model using machine learning and deep learning to precisely determine when adaptive radiotherapy (ART) should be triggered, providing a valuable tool for personalized precision cervical cancer treatment. The research has been published in the prestigious International Journal of Radiation Oncology-Biology-Physics. It was backed by China’s National Key R&D Program and the National High Level Hospital Clinical Research Funding.
Cervical cancer remains one of the common malignancies to women worldwide, making treatment precision a top clinical priority. For patients with locally advanced cervical cancer, concurrent chemoradiation is the first-line curative treatment approach. However, pelvic organs constantly shift due to natural factors like bladder filling and intestinal gas, causing tumor targets to move and change shape between treatment sessions. This creates a major hurdle for delivering precision radiation therapy.
ART offers a promising solution. This approach allows medical teams to tailor treatment plans in real-time, adjusting radiation delivery based on daily imaging to offer truly personalized therapy for each patient. However, each ART session takes over 20 minutes on average, requiring substantial medical resources and time investment. This limits how widely the technology can be adopted in clinical practice. Currently, doctors have to make subjective decisions about when to use ART based on daily scans, which leads to not only inter-observer variability but also inefficient decision-making.
Directors Zhang Fuquan and Hu Ke's teams have tackled this problem head-on by bringing artificial intelligence (AI) into the equation. Their AI model harnesses both machine learning and deep learning algorithms to analyze daily imaging data, examining morphologic, gray-level, and dosimetric features. The system can then intelligently predict the optimal moments to trigger ART.
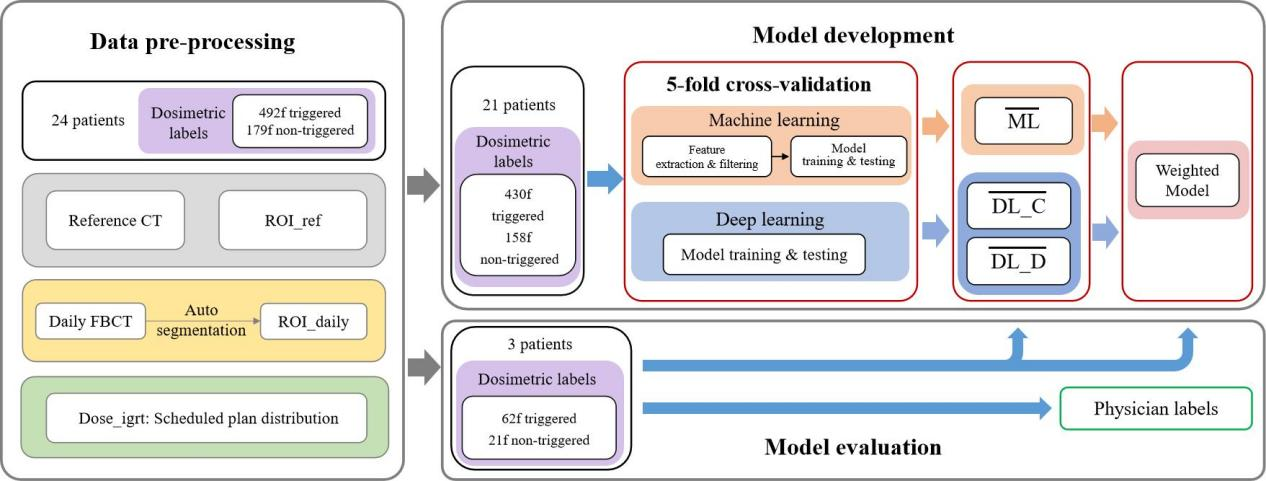
▲Development and evaluation workflow for the AI-powered ART decision system
According to the research results, the machine learning-based model achieved accuracy, precision, and recall of 0.825, 0.824, and 0.827, respectively. But the deep learning-based model delivered even better results, with accuracy, precision, and recall of 0.869, 0.860, and 0.881, respectively. Evaluation on an independent data set shows that the AI model is more robust, with its prediction accuracy significantly outperforming the physician consensus (0.855 vs 0.795).
This breakthrough extends far beyond enhancing cervical cancer ART precision – it represents a smart approach to healthcare resource management. As Director Hu Ke explains, the AI model enables more precision treatment for patients and eliminates unnecessary resource waste, delivering gains in both accuracy and efficiency.
Co-first authors of this paper: Dr. Sun Shuai, Associate Chief Physician in the Department of Radiotherapy, and Gong Xinyue, a Class 2018 doctoral candidate in the Eight-Year Program of Clinical Medicine.
Written by Sun Shuai and Gong Xinyue
Picture courtesy of Sun Shuai and Gong Xinyue
Reviewed by Hu Ke
Edited by Dong Jingge
Chief editor Duan Wenli
Supervised by Wu Peixin
