Recently, the "British Journal of Haematology" (JCR Q1) published as an original paper the latest research outcomes of the hematology team at PUMCH. The study innovatively revised the definition of idiopathic plasmacytic lymphadenopathy (IPL), considering it a distinct subtype of idiopathic multicentric Castleman disease-not otherwise specified (iMCD-NOS). The study analyzed the unique demographics, clinical features, treatment regimens, and prognosis of this subtype, likely to revise the existing classification of idiopathic multicentric Castleman disease (iMCD).
iMCD is a group of rare blood diseases characterized by systemic inflammatory symptoms, and it was included in China’s first rare disease catalog. According to the current international consensus, iMCD is further classified into iMCD-thrombocytopenia, anasarca, fever, reticulin fibrosis and organomegaly (iMCD-TAFRO) and iMCD-NOS. The two groups differ remarkably in clinical manifestations, therapeutic responses and prognoses. iMCD-NOS, as defined under the current classification framework, comprises a diverse collection of diseases with widely varying clinical manifestations, therapeutic responses and prognoses. This suggests the need for further subclassification. The definition of IPL, a subtype of iMCD with unique manifestations, and how it fits in the iMCD classification framework remain controversial.
The PUMCH team tried to further classify iMCD-NOS patients. Having compared the rationality of past definitions of IPL, they made innovative revisions of the definition (serum immunoglobulin G (IgG) level >17.4g/L, mixed or plasmacytic pathological type, and platelet count >350*10^9/L). Based on this revised definition and the new positioning, the research team utilized the largest retrospective cohort to date to compare the clinical characteristics and outcomes of iMCD-IPL and iMCD-NOS w/o IPL patients within the current international consensus framework for iMCD-NOS.
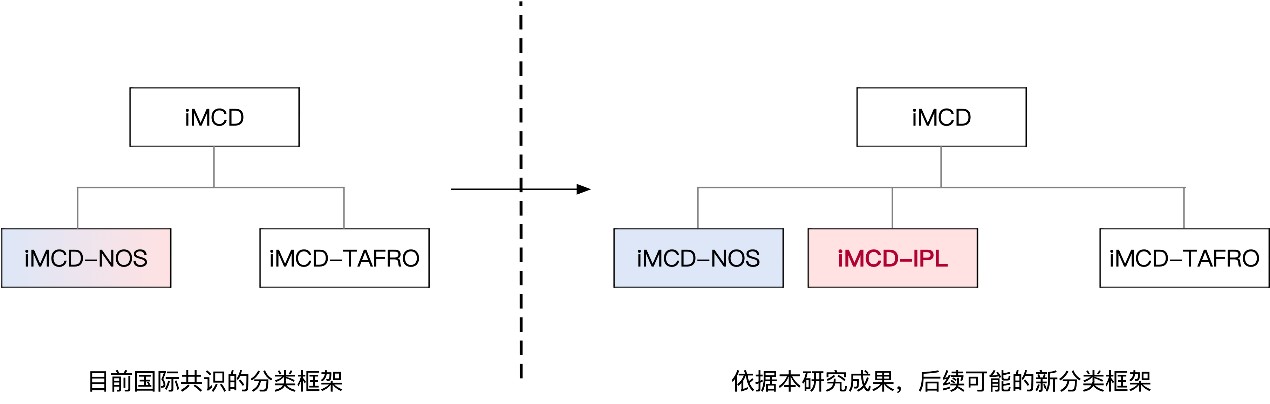
▲Figure 1. Clinical subtypes of iMCD (left: current international consensus; right: possible revised framework based on this study)
Compared with patients with iMCD-NOS w/o IPL, iMCD-IPL patients were younger when diagnosed and presented with more severe inflammatory symptoms, but were less likely to develop renal impairment and had significantly better overall survival (see Figure 2). When the iMCD international severity classification system was used to classify them, there were no significant differences between the two groups, further suggesting the uniqueness of the IPL subtype. In terms of treatment, patients of iMCD-IPL and patients of iMCD-NOS w/o IPL exhibited significant differences in sensitivity to treatment regimens. Compared with lymphoma-like treatment strategy, patients with iMCD-IPL benefitted more from a multiple myeloma-like and IL-6-blocking treatment strategy, which were associated with a higher response rate and, importantly, a longer median TTNT (time to next treatment), while no differences were observed in non-IPL patients. This study aids in a deeper understanding of the disease, informs treatment, and improves prognosis, providing guidance for clinical practices.
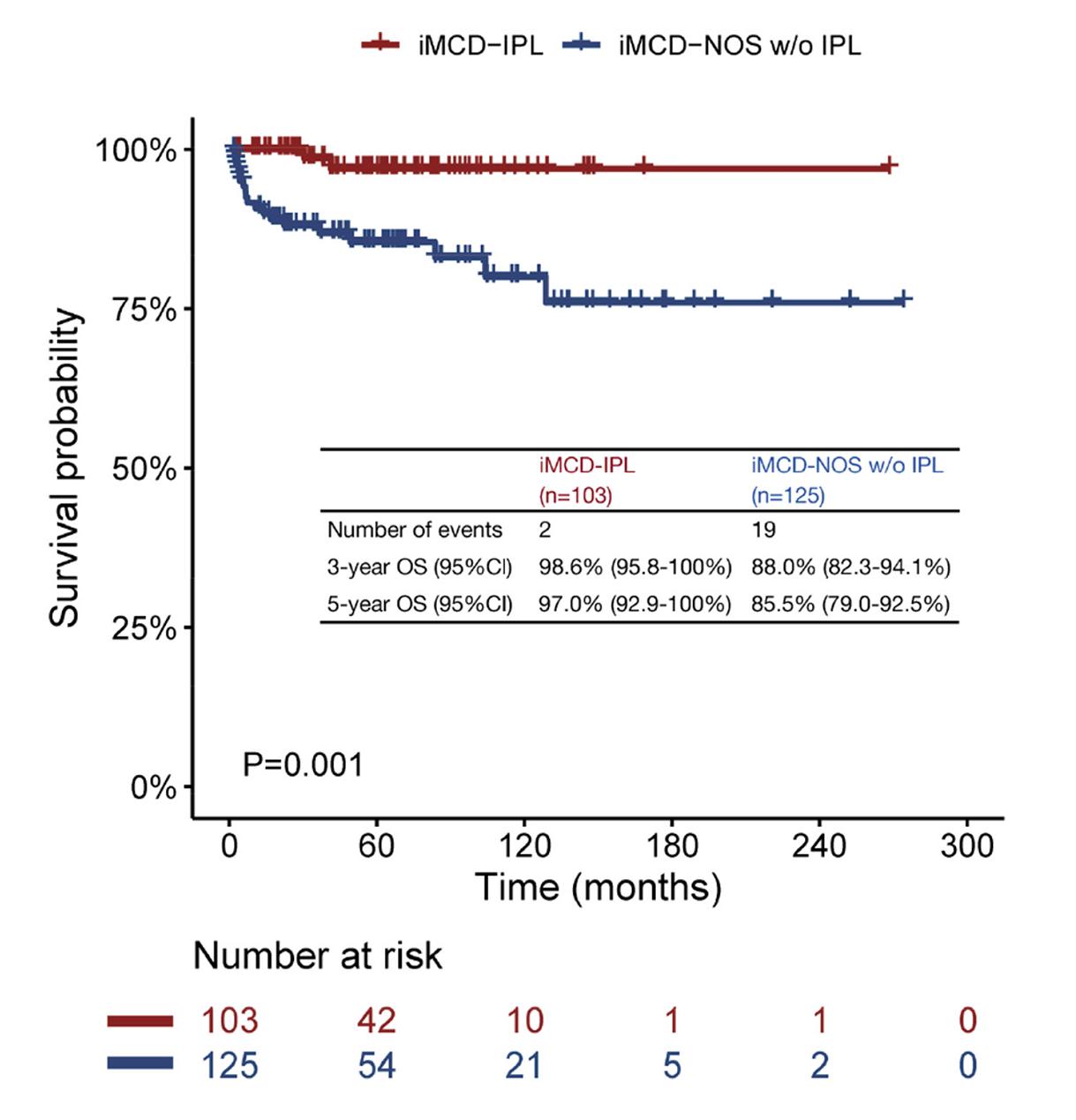
▲Figure 2. The prognosis of iMCD-IPL patients was significantly better than that of iMCD-NOS patients
Written by the Department of Hematology and the Publicity Department
Pictures courtesy of the Department of Hematology
Edited by Yan Xiaobo and Chen Xiao
Translated by Liu Haiyan
Reviewed by Zhao Danqing and Wang Yao
