Recently, the pathology team led by Chen Jie from the pathology Ddepartment of Pathology PUMCH published a papertheir latest work in “Modern Pathology” (a tier 1 journal, or among the top 5%, as ranked by the Chinese Academy of Sciences). The paper analyzed the clinicopathological characteristics and clinical prognosis of 486 cases of solid pseudopapillary neoplasms of the pancreas (SPN). The team has also established a preliminary risk prediction model for SPN. This research was supported by the National High LevelHigh-Level Hospital Clinical Research Funding.
SPN is generally considered to be a a low-grade malignancy with a low incidence rate.. Most cases can be cured through by surgical resection, but a small proportion of patients may experience recurrence, metastasis, or even death, with reported metastasis rates ranging from 10% to 15%. In recent years, the increasing prevalence of various abdominal imaging modalities has resulted in a noticeable rise in its incidence (discovery).
This research retrospectively admitted enrolled 486 SPN patients diagnosed at PUMCH. Follow-up data was available for 438 patients (90.1%), and the median follow-up time was 58.5 months (1-334 months). Among the follow-up patients, one died of prolonged malnutrition after the surgery, and 26 experienced recurrence or metastasis (including synchronous metastasis). The follow-up showed that the overall survival and disease-specific survival rates were 99.8% and 100%, respectively. The study found significant differences in various dimensions aspects such as symptoms, tumor size, pathological T staging, lymph node metastasis, extratumoral lymphointravascular embolivascular invasion, and Ki-67 index between the 460 patients without recurrence or /metastasis and the 26 patients with recurrence/metastasis. The differences are statistically significant.
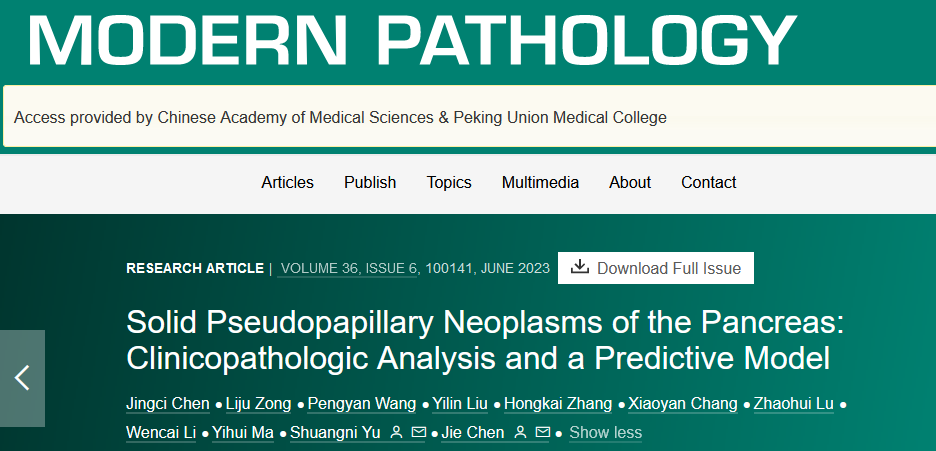
▲Representative images of lymphovascular invasion (LVI)
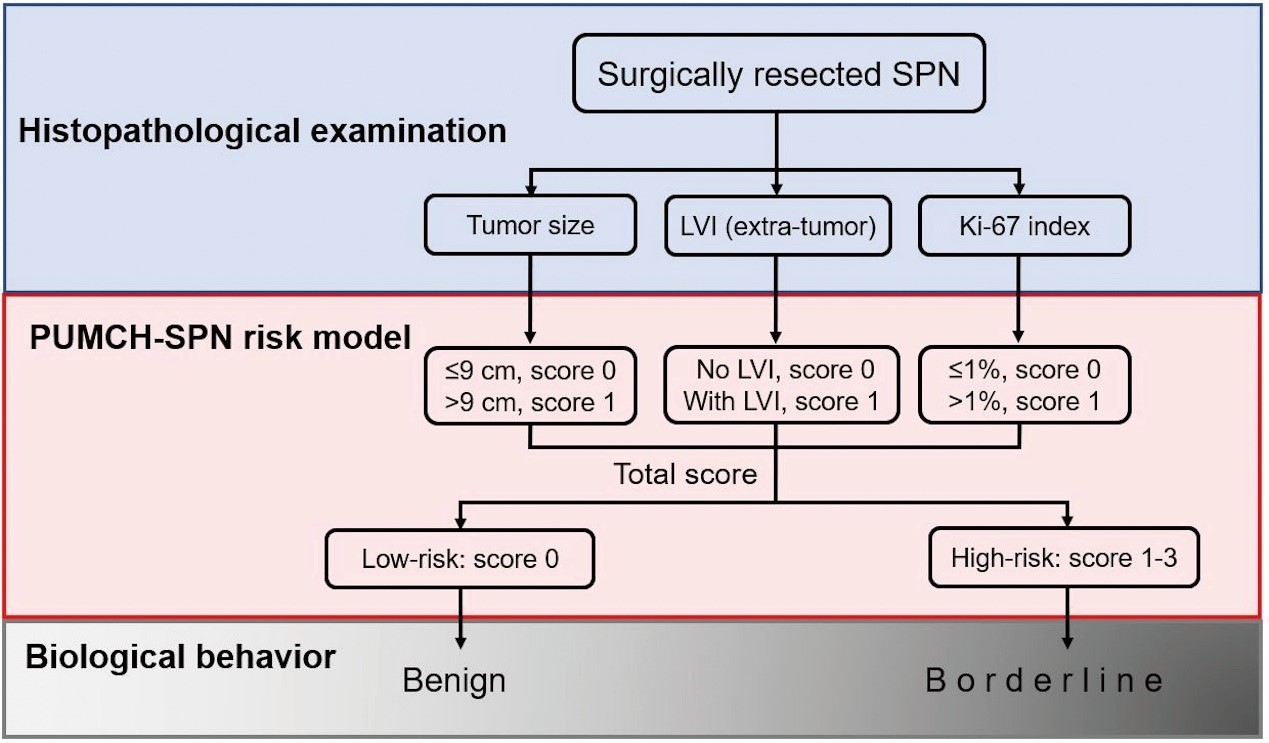
MA multivariate analyseis showed that tumor size (>9cm), the presence of lymphovascular invasion status (presence), and a the higher Ki-67 index (>1%) were three independent predictors of SPN progression. On the basis ofBased on that, a PUMCH-SPN risk model was built developed to evaluate the risk of relapse and it was compared with the American Joint Committee on Cancer tumor staging system (AJCC, the eighth edition). The PUMCH-SPN model demonstrated a higher sensitivity for screening SPN patients with a high risk of relapse/metastasis.

▲Comparison between the relapse risk-predicting PUMCH-SPN model and the AJCC staging systemmodel
The researchers further obtained data from 116 cases and 72 cases of SPN from the PubMed database and other hospitals in China, respectively, as external validation cohort for the PUMCH-SPN risk prediction model, which was found to be stable and effective, with a sensitivity of 98.3%.
As the behind-the-scenes “judge”, the pathology department plays a crucial role in clinical practices. This study indicates that using tthe PUMCH-SPN risk prediction model can classify SPN into low-risk and high-risk groups in a simple and clear mannersimply and clearly, and thus helps helping predict SPN prognosis and develop more rational follow-up plans.
Written by Gan Dingzhu and Chen Jingci
Translated by Liu Haiyan
Reviewed by Lu Junliang and Wang Yao
