Recently, Professor Liu Xiaoqing’s team from the Department of Infectious Diseases at PUMCH published their clinical research findings on latent tuberculosis infection (LTBI) and its associated factors in patients with systemic lupus erythematosus (SLE) in “Microbiology Spectrum” (a tier 1 journal, or among the top 5%, as ranked by the Chinese Academy of Sciences). This study is based on a multicenter cross-sectional study conducted in tertiary general hospitals in China. The study screened for LTBI among patients with SLE using the T-SPOT.TB assay and identified factors affecting the assay results. This research was supported by the National High Level Hospital Clinical Research Funding.
SLE is a rheumatic immune disease with the most complex pathogenesis, the most prominent multi-organ involvement, the strongest clinical heterogeneity, and the highest proportion of patients. China has approximately 1 million SLE patients, with an estimated prevalence of 30/100,000 to 70/100,000, ranking second in the world. When SLE is combined with active tuberculosis (ATB), the clinical symptoms are often atypical, leading to missed diagnosis or misdiagnosis. Such patients tend to be severely ill and have a high mortality rate. Active screening and preventive intervention for LTBI in SLE patients will effectively reduce the incidence rate, mortality rate, and transmission risk of ATB, as well as medical costs, bringing about significant health and social benefits.
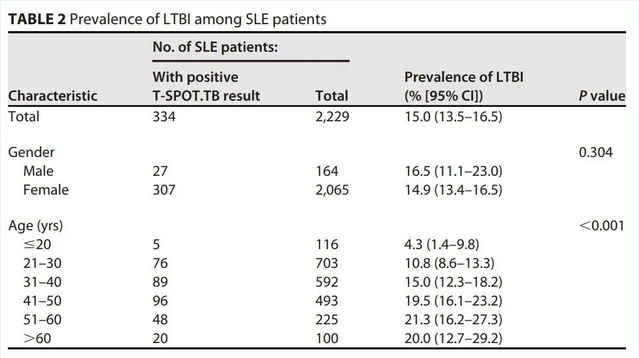
▲Proportion of positive T-SPOT.TB results
Multivariable logistic regression analysis showed that patients over 40 or with evidence of previous tuberculosis were more likely to have positive T-SPOT.TB results, while patients with a SLEDAI-2K score of ≥10, a glucocorticoid dose of ≥60 mg/d, leflunomide (LEF) treatment, or tacrolimus (FK506) treatment were more likely to have negative T-SPOT.TB results. Further analysis showed that in patients with a SLEDAI score ≤4, a glucocorticoid dose<30 mg/d, and no LEF or FK506 at baseline, the positivity rate of T-SPOT.TB in SLE patients was 20.6%. For SLE patients who did not use steroids under the aforementioned conditions the positive rate of T-SPOT.TB was 24.5%.
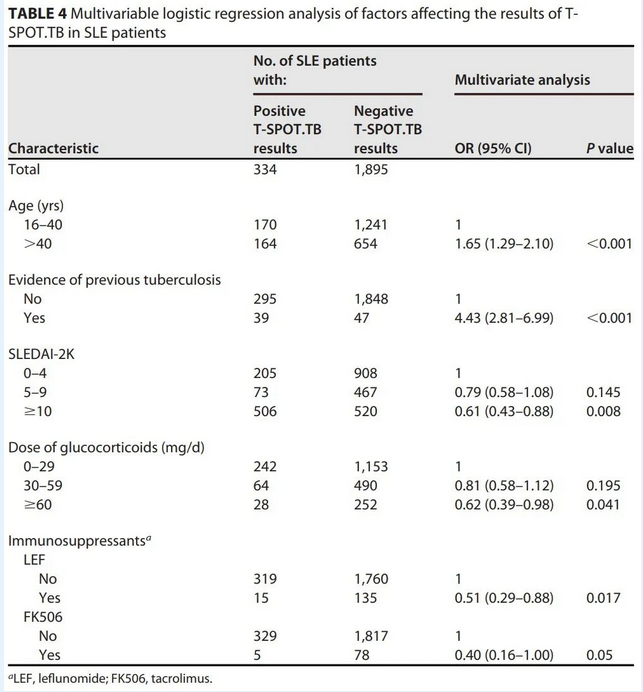
▲Multivariable logistic regression analysis of factors affecting the results of T-SPOT.TB in SLE patients
This study found that the prevalence of LTBI in SLE patients, with T-SPOT.TB as the screening method, was about 15%. In patients with mid-to-high disease activity, high-dose glucocorticoids, and treatment with LEF and tacrolimus, there is the possibility of false negatives in SLE patients with T-SPOT.TB. This suggests that clinicians, while currently primarily using immunological diagnostic methods to screen for LTBI, should pay attention to the possibility of false negative results. When screening for LTBI in SLE patients with different immune statuses, a combination of multiple screening methods and a more personalized risk assessment should be considered.
Translated by Liu Haiyan
Reviewed by Zhang Lifan and Wang Yao
