Recently, Professor Xiao Yi and his team from the Department of Respiratory and Critical Care at PUMCH published an original article in the “Annals of the American Thoracic Society” (Tier 1, or among the top 5%, as ranked by the Chinese Academy of Sciences). Their study utilized an innovative index developed by the team called the Sleep Breathing Impairment Index (SBII) to assess the association between co-morbid obstructive sleep apnea (OSA) and insomnia and incident diabetes in a population. The study found that patients with co-morbid OSA and insomnia had a significantly higher risk of developing incident diabetes. This conclusion provides a theoretical basis for the early identification and intervention of diabetes in patients with sleep disorders.
Patients with OSA have a higher risk of developing type 2 diabetes due to nocturnal hypoxia and fragmented sleep. Insomnia patients experience repeated sympathetic nervous system activation during the night, which is also a high-risk factor for type 2 diabetes. Patients with co-morbid OSA and insomnia, as a specific subgroup with sleep disorders, have significantly higher risks of cardiovascular and cerebrovascular diseases as well as neurocognitive disorders. However, the association between this subgroup and type 2 diabetes is still inconclusive.
In this study, a retrospective cohort design was employed using sleep research data from a cohort of US male with osteoporotic fractures. During a median follow-up of 10 years, the incidence of type 2 diabetes was tallied. Survival analysis and model construction were conducted to identify patients with co-morbid OSA and insomnia (COMISA) based on the Sleep Breathing Impairment Index (SBII) and Apnea Hypopnea Index (AHI) respectively. The study compared the relationship of these two subgroups with incident diabetes, and the predictive value of COMISA-SBII (COMISA based on SBII) and COMISA-AHI (COMISA based on AHI) for type 2 diabetes respectively.
The final analysis included 2,365 community-dwelling men (mean age 76 years) without diabetes at baseline. During a median follow-up of 10.0 years, 181 developed diabetes. Participants with COMISA-SBII had a higher risk of incident diabetes than those without sleep disorders. And the results remained significant after adjusting for demographics, comorbidities, smoking and alcohol consumption behavioral risk factors, and death as a competing risk.
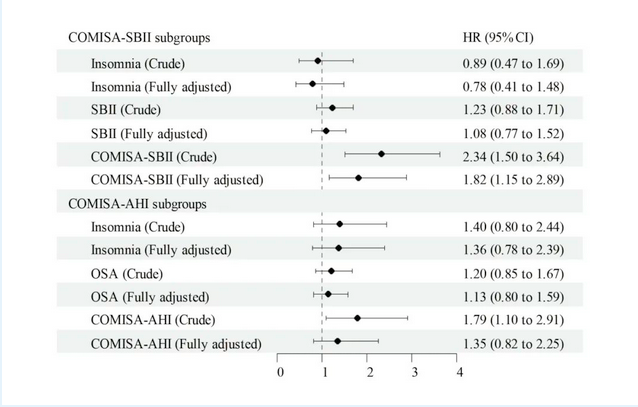
▲The survival analysis of the COMISA-SBII subgroups and the COMISA-AHI subgroups and their risks of incident diabetes
The results show that the type 2 diabetes risk model based on SBII has higher values of AIC, BIC, concordance index, IDI, and NRI for predicting incident diabetes than the model based on AHI. This suggests that the predictive model based on SBII has better goodness of fit and predictive accuracy.
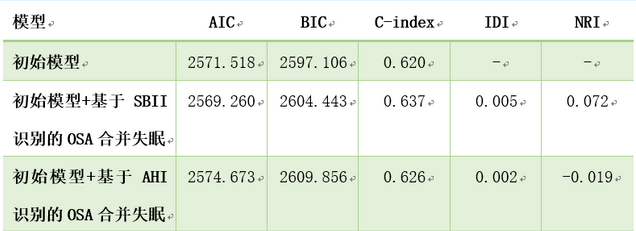
▲Comparison of predictive performance between the clinical model based on SBII and AHI. The initial model for predicting incident diabetes includes variables such as age, BMI > 30, hypertension, cardiovascular disease, smoking, and alcohol consumption
These study findings indicate that patients with COMISA have a significantly increased risk of developing type 2 diabetes. For such patients, active intervention for OSA and insomnia, such as continuous positive airway pressure (CPAP) therapy and cognitive-behavioral therapy, should be pursued. Regular assessment of glucose metabolism is also recommended to beware the occurrence of glucose metabolic disorders and type 2 diabetes.
Written by Guo Junwei and Yan Xiaobo
Pictures courtesy of the Department of Respiratory and Critical Care
Edited by Yan Xiaobo and Chen Xiao
Reviewed by Tian Xinlun and Wang Yao
