Recently, “Chest” (a Tier 1 journal, or among the top 5%, as ranked by the Chinese Academy of Sciences) published the research results of Prof. Xu Kai-Feng’s team from the Department of Pulmonary and Critical Care Medicine of PUMCH as Original Article. By analyzing data from the clinical cohort of lymphangioleiomyomatosis (LAM) in PUMCH, the study revealed the key determinants of the progression and survival prognosis of LAM. The study showed that the blood biomarker vascular endothelial growth factor D (VEGF-D) was associated with disease progression and survival prognosis, and that rapamycin (sirolimus) not only slowed down disease progression, but also significantly improved the survival prognosis of LAM patients. This study was supported by the National High Level Hospital Clinical Research Funding.
LAM is a rare disease almost exclusively seen in women and characterized by progressive diffuse cystic lesions of the lungs, with the 10-year survival rate at approximately 85%. It was included in the first catalog of rare diseases in China. Recent years saw two major progresses for LAM, namely development of rapamycin, the first effective drug, and establishment of VEGF-D as a diagnostic biomarker. The multidisciplinary team led by Prof. Xu Kai-Feng has conducted long-term follow-up observations and studies on LAM clinical cohorts. In this study, 2 datasets were retrieved from the PUMCH LAM Cohort, namely the progression dataset of 282 patients and the survival dataset of 574 patients.
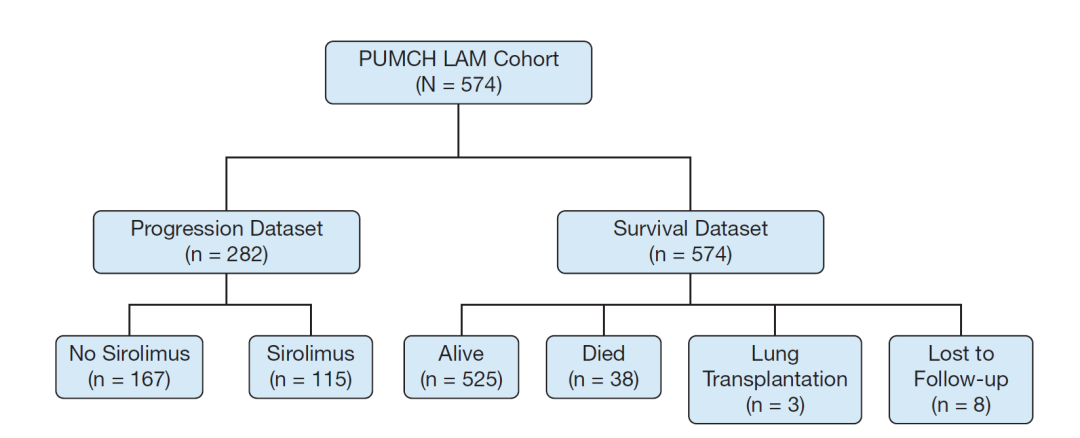
▲Flow chart of the study
The patients in the progression dataset were divided into a no sirolimus treatment group (n = 167) and a sirolimus group (n = 115). The study showed that rapamycin was effective in slowing the decline in lung function measured by FEV1.
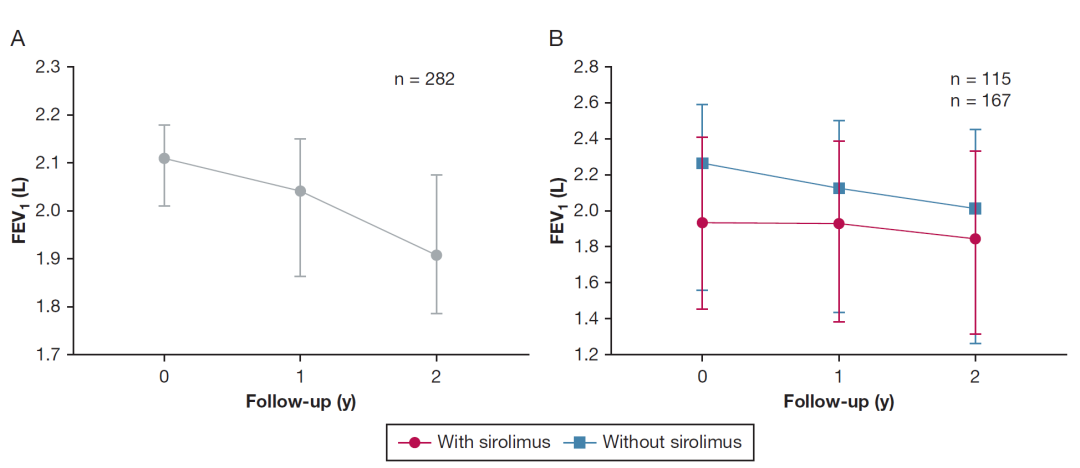
▲The change in FEV1 (forced expiratory volume in 1 second) of LAM patients at the two-year follow-up (A. All patients; B. The group with sirolimus treatment and the group with no sirolimus treatment)
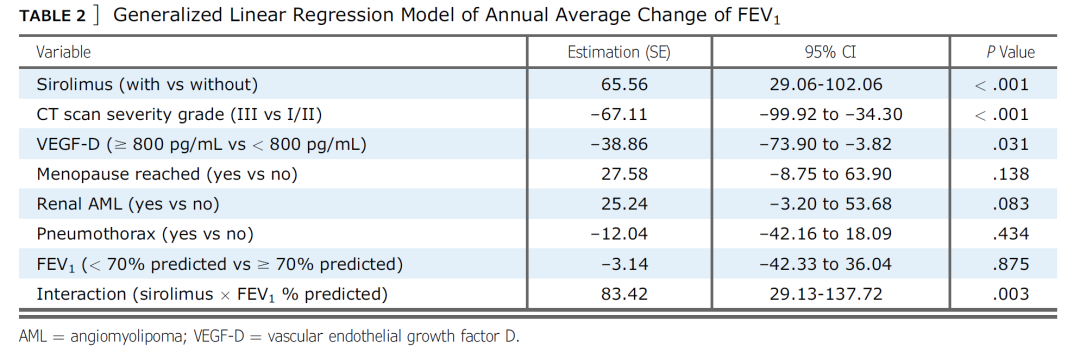
Analysis of the disease progression cohort using the generalized linear model identified 3 key factors strongly associated with changes in FEV1, an indicator of disease progression, namely “sirolimus, CT scan severity grade and VEGF-D” (see the table below). Other factors, such as “menopause reached”, “renal AML” and “pneumothorax” were not significantly associated with changes in baseline FEV1.
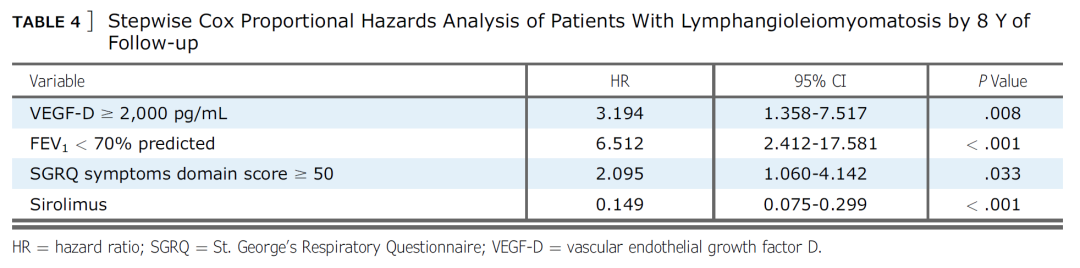
According to data of the survival cohort, the cumulative survival rates at 5 years and 8 years after the initial evaluation were 92.2% and 87.1%, respectively. The 8-year cumulative survival rates in the sirolimus and no sirolimus groups were 89.9% and 78.4%, respectively. The 8-year cumulative survival rates of patients with baseline FEV1 of ≥ 70% predicted and baseline FEV1 of < 70% predicted were 95.5% and 80.6%, respectively. The 8-year cumulative survival rates of patients with VEGF-D of ≥ 2,000 pg/mL and VEGF-D of < 2,000 pg/mL were 82.9% and 95.1%, respectively. The 8-year survival rates for patients with SGRQ symptoms domain scores of ≥ 50 and SGRQ symptoms domain scores of < 50 were 79.89% and 90.91%, respectively.
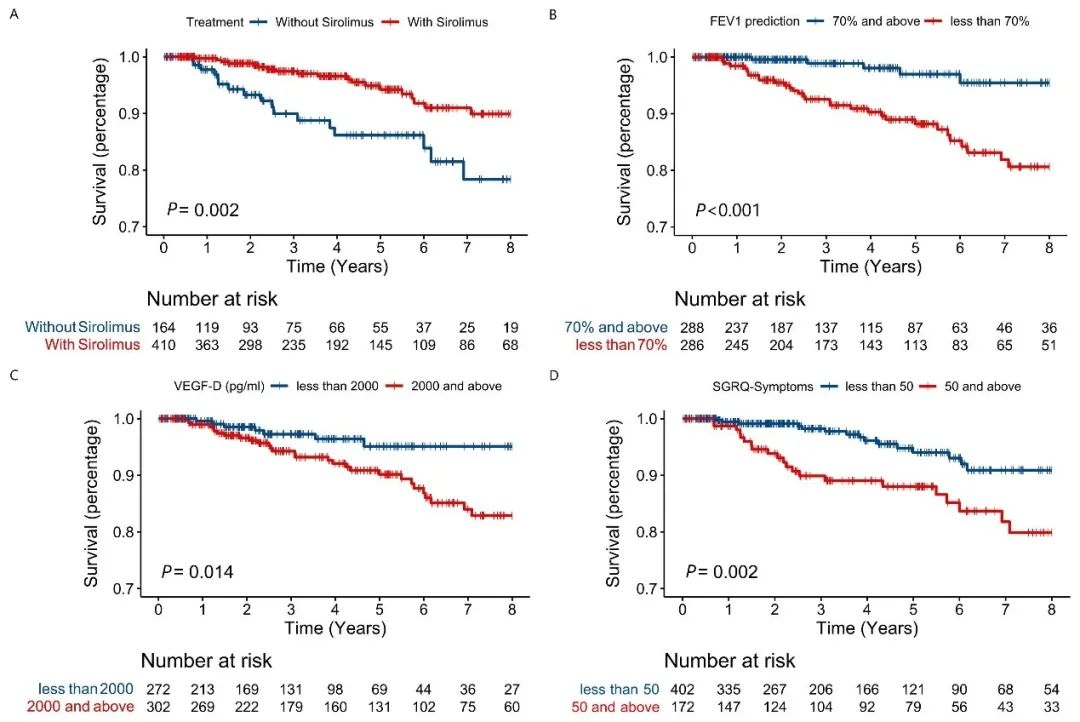
▲Kaplan-Meier survival curves for LAM patients: A. Survival curves by sirolimus treatment status; B. By FEV1 % predicted; C. By VEGF-D levels; D. By the SGRQ symptoms domain score (SGRQ = St. George’s Respiratory Questionnaire)
In stepwise Cox proportional hazards analysis of patients with LAM, the risk of death or lung transplantation was 85.1% lower in patients treated with sirolimus, was 2.194 times higher in patients with VEGF-D levels of ≥ 2,000 pg/mL than in patients with VEGF-D levels of < 2,000 pg/mL, and was 5.512 times higher in patients with baseline FEV1 of < 70% predicted than in patients with FEV1 of ≥ 70% predicted (see the table below). The risk of death in the sirolimus group decreased by 85.6% after inverse probability of treatment weighting analysis.
The most significant findings of this study: first, serum VEGF-D, as a biomarker of LAM, was associated with disease progression and survival prognosis; second, rapamycin, as a therapeutic agent for LAM, not only effectively slowed down the disease progression, but also significantly improved the survival prognosis of LAM patients.
Written by the Department of Pulmonary and Critical Care Medicine
Pictures courtesy of the Department of Pulmonary and Critical Care Medicine
Edited by Yan Xiaobo and Chen Xiao
Translated by Liu Haiyan
Reviewed by Tian Xinlun and Wang Yao
