Recently, the New England Journal of Medicine published an article online on the treatment of COVID-19 by lopinavir/ritonavir (Aluvia). The conclusion of the article showed that Aluvia did not see obvious efficacy in the treatment of COVID-19 patients, which confirmed that up to now, there is no effective antiviral treatment for SARS-CoV-2 infection patients. On March 20, 2020, an article by professor Taisheng Li and Wei Cao as corresponding authors was published online on Emerging Microbes & Infections (EMI, impact factor 6.212), which is titled " Hypothesis for potential pathogenesis of SARS-CoV-2 infection — a review of immune changes in patients with viral pneumonia". This article is the first to discuss the potential pathogenesis of the novel coronavirus, and it is recommended that intravenous immunoglobulin (IVIG) combined with low molecular weight heparin (LMWH) anticoagulation therapy is one of the important therapeutic strategies for severe COVID-19 patients.
COVID-19 is pandemic now. Treatment of severe and critical illness is crucial to the reduction and control of fatality. In China,managing the current severe and critical illness and further reducing the fatality rate is still a top priority. As early as late January, professor Taisheng Li’s team from the Department of Infectious Medicine of Peking Union Medical College Hospital began to study the pathogenesis, course of disease and treatment.
Basing on the published literature and clinical observations of COVID-19 patients, authors propose reasonable hypotheses about the pathogenesis of SARS-CoV-2 infection in humans.
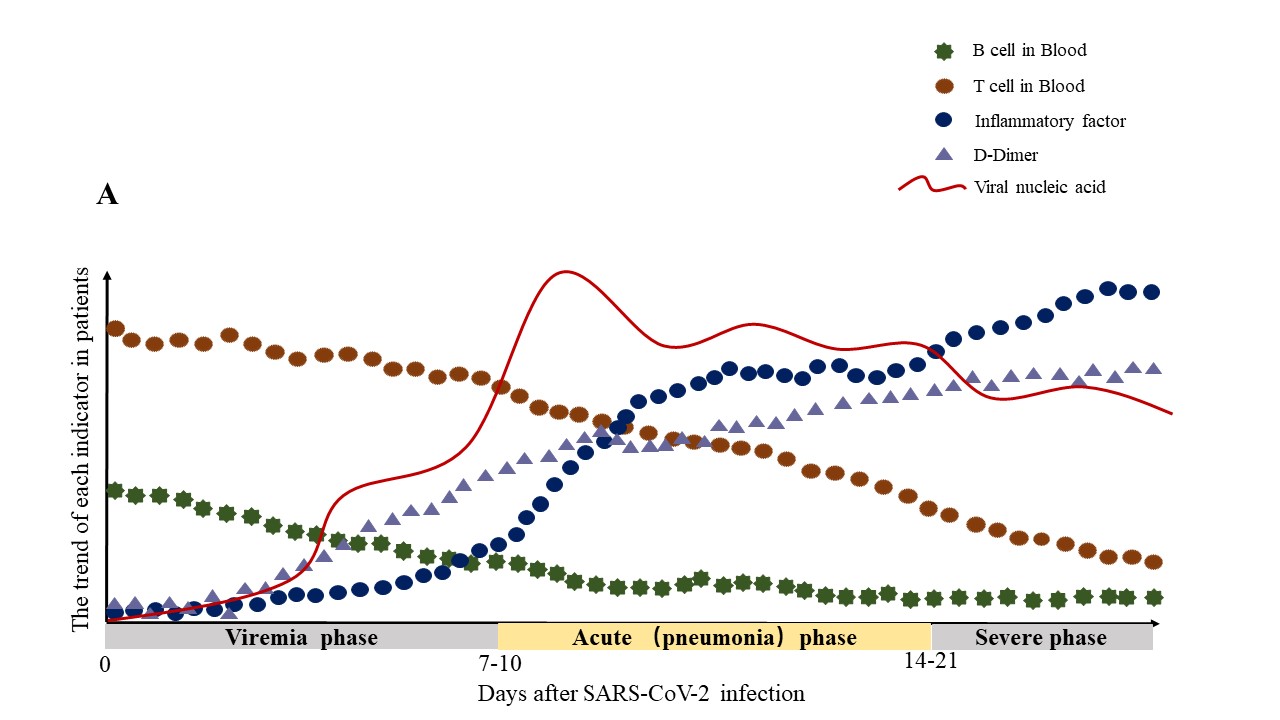
The virus might pass through the mucous membranes, especially nasal and larynx mucosa, then enters the lungs through the respiratory tract. The early most common symptoms of infection are fever and cough. The virus may enter the peripheral blood from the lungs, causing viremia. Then the virus would attack the targeting organs that express ACE2, such as the lungs, heart, kidneys, gastrointestinal tract. The SARS-CoV-2 detected in the fecal samples is more likely because the virus enters the blood from the lungs and then travels from the blood to the intestines, which supports the author’s hypothesis. The median time from symptom onset to ARDS was about 8 days. The authors speculate that in this way, the virus begins a second attack, causing the patient’s condition to aggravate around 7 to 14 days after onset. During the infection process, the white blood cell count in peripheral blood in the early stage of the disease is normal or slightly low, and lymphopenia is observed in patients. Authors speculate that B lymphocyte reduction may occur early in the disease, which may affect antibody production in the patient. In severe type patients, lymphocytes were significantly reduced. The authors speculate that lymphocytes in patients with COVID-19 might gradually decrease as the disease progress. But the mechanism of significant lymphocyte reduction in severe type patients remains unclear. Besides, the inflammatory factors associated with diseases mainly containing IL-6 significantly increased, which also contributed to the aggravation of the disease around 7 to 14 days after onset. Non-survivors had higher levels of neutrophils, D-Dimer, blood urea nitrogen, and creatinine than the survivors.
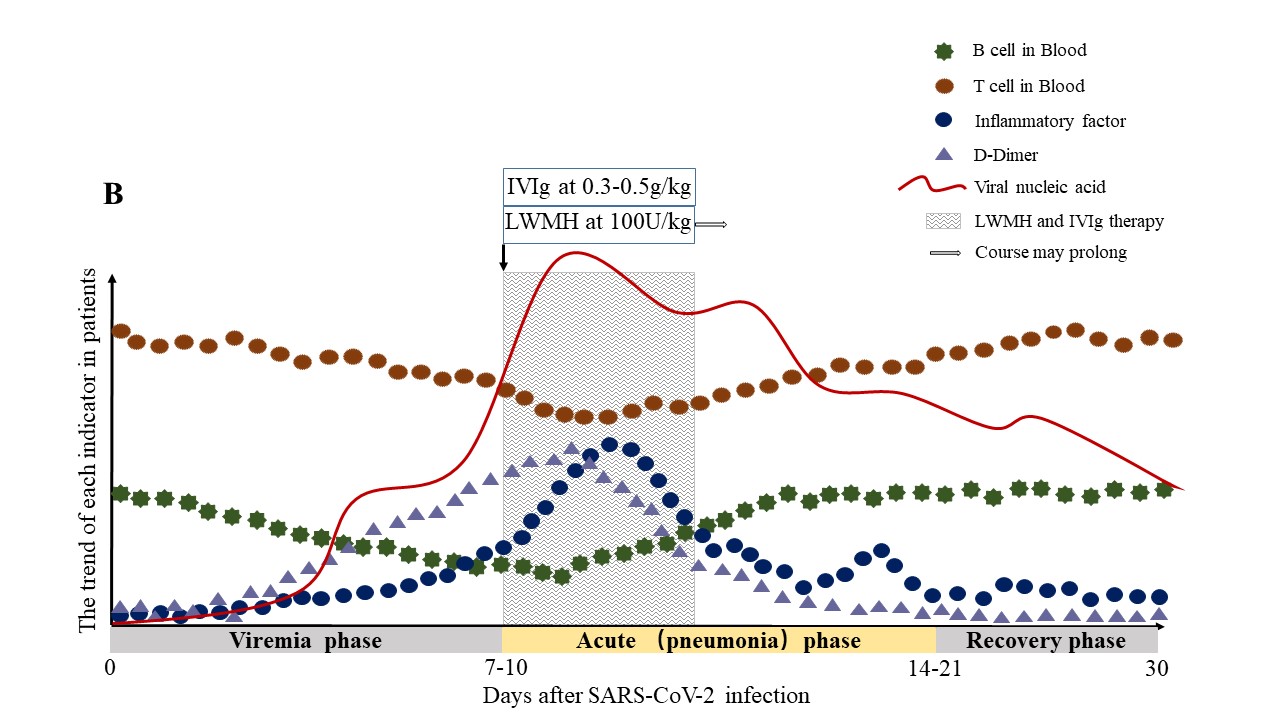
Based on the above assumptions, the clinical phase is divided into three: the viremia phase, the acute phase (pneumonia phase), and the recovery phase.
If the immune function of patients in the acute phase (pneumonia phase) is effective, and no more basic diseases, the virus can be effectively suppressed, then enter the recovery phase. If the patient is older, or in an immune impaired state, combined with other basic diseases such as hypertension and diabetes, the immune system cannot effectively control the virus in the acute phase (pneumonia phase), the patient will become severe or critical type. To enhance the immune function of patients and inhibit the formation of inflammatory factor storms, authors recommend early initiation of IVIG and LMWH anticoagulant therapy, which is effective in improving the prognosis of severe and critical illness. Authors have observed in clinical that COVID-19 patients with severe type may develop disseminated intravascular coagulation (DIC). The article recommends that high-dose IVIG at 0.3-0.5g per kg weight per day could be given for 5 days. The recommended dose of LMWH is 100U per kg weight per 12 hours by subcutaneous injection for at least 3-5 days. The article suggests that IVIG and LMWH anticoagulantion therapy could be given as early as possible when T cells, B cells, inflammatory cytokines, and D-Dimer show the following trends: T lymphocytes and B lymphocytes in peripheral blood significantly decreased; inflammatory cytokines such as IL-6 notably increased; coagulation parameters such as D-Dimer abnormally increased; Chest CT indicating the expansion of lung lesions.
More IVIG and anticoagulant effects are currently being summarized. Besides, immune system changes have always played an important role in the development of infectious diseases. To further understand the diseases, advance therapeutic strategies and improve prognosis, more immune research on COVID-19 should be carried out.
https://doi.org/10.1080/22221751.2020.1746199
Writer: Ling Lin
Photo: Department of Infectious Diseases, PUMCH
