
On September 6, 2024, Professor Zhu Lan's team from PUMCH, in collaboration with BGI Research and others, published an article online in Nature Communications (IF=16.6), a journal within the Nature portfolio. The study elucidates the assembly process of the neovaginal microbiota in patients with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome following laparoscopic peritoneal vaginoplasty, providing important scientific evidence for improving the vaginal microbiota in these patients.
The vaginal microbiota, comprising an abundance of microorganisms colonizing the female vagina, is crucial in the human body. It plays a vital role in maintaining vaginal health and protecting the host from diseases. MRKH syndrome is a rare congenital disorder characterized by uterovaginal agenesis in females. Vaginoplasty is an important treatment method for MRKH syndrome. During surgery, a canal between the urethra, bladder and rectum was created and lined with dissected peritoneum, intestine, or biological grafts. In this way, the neovaginal cavity was created. The neovagina provides a unique model that allows researchers to analyze the de novo assembly and evolution of the vaginal microbiota in adult women from fresh perspectives, thereby enhancing our understanding of the assembly mechanisms.
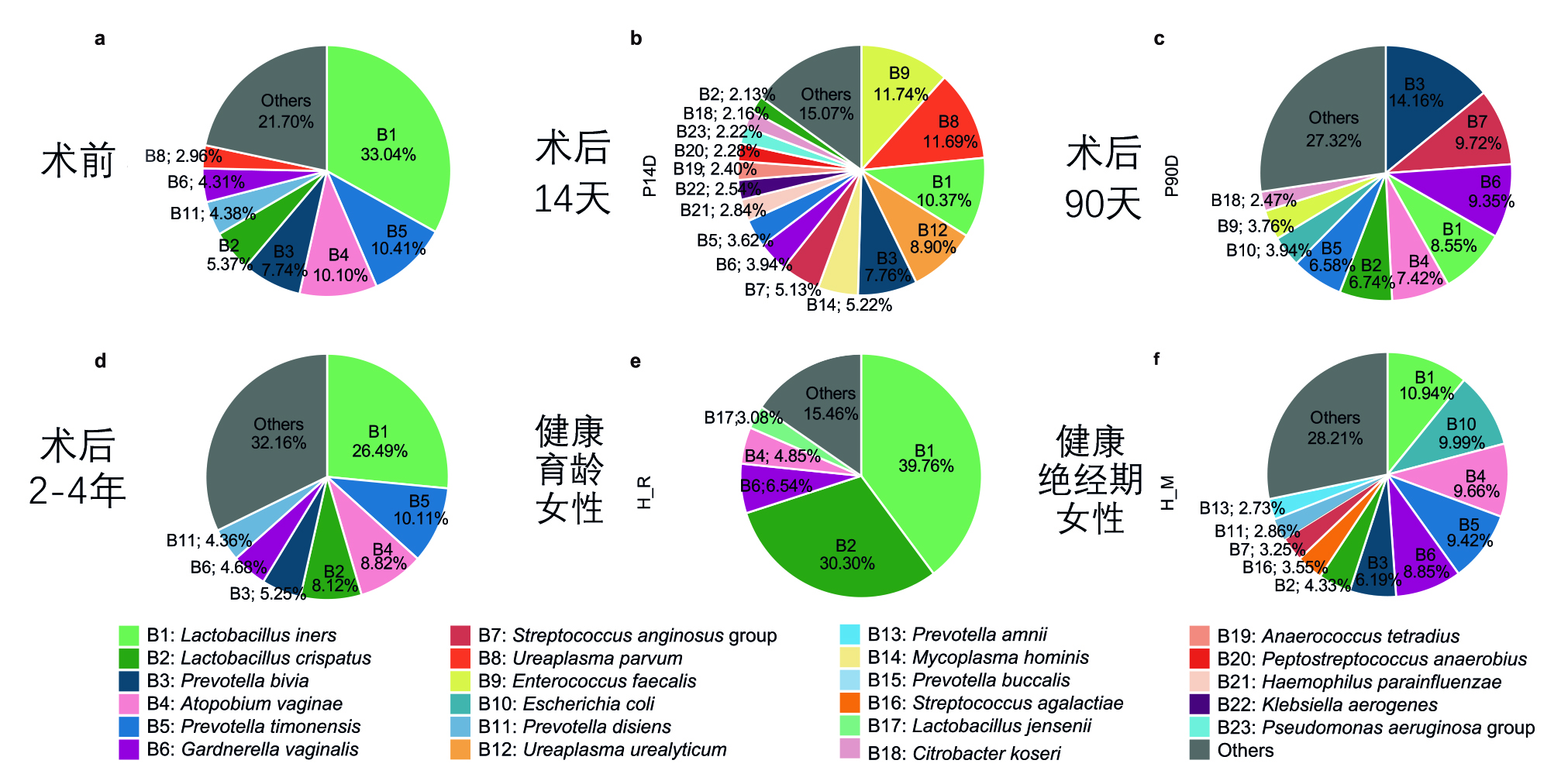
▲Compositional developments along the assembly of the microbiota in the neovagina in MRKH patients pre-surgery and post-surgery, and in comparison with healthy women
The study results show that when initially created, the neovagina represents a nearly blank ecological niche, with the microbiota of the dimple and the anus area, among other adjacent anatomical regions, constituting the primary species pools. Post-surgery, the local environment of the neovagina undergoes dynamic transformation: The original dimple, acting as the neovaginal opening post-surgery, formed the initiating site for spontaneous upward squamous epithelization in the neovagina, which gradually covered the initial peritoneal tissues and formed structural tissues the same as those of normal female vaginas. The nutritional conditions of the neovagina also transitioned from "extremely barren" to "relatively barren" (similar to menopausal conditions) and finally to "sufficient" (comparable to women of reproductive age).
Under the combined influence of the "species pool" and environmental selection, the vaginal microbiota also undergoes continuous changes. The neovaginal microbiota 14 days post-surgery exhibited stochastic characteristics, with significant individual differences and notable proliferation of some drug-resistant bacteria. Three months post-surgery, the microbial community began to evolve towards a normal vaginal microbiota structure, similar to that of healthy menopausal women, with a low level of Lactobacillus and coexistence of various anaerobic bacteria. As nutritional conditions gradually improved, the neovagina began to resemble that of healthy women of reproductive age, with Lactobacillus abundance progressively increasing. At 2-4 years post-surgery, it had further evolved into a structure closely resembling the homeostatic pre-surgery dimple microbiota.
The study also found that Lactobacillus crispatus colonizing the neovagina, one of the most important probiotics in healthy women, primarily originated from the pre-surgery vaginal dimple. This suggests that introducing Lactobacillus crispatus before surgery or in the early post-operative period might help promote the colonization of this probiotic and facilitate the rapid formation of a healthy and stable vaginal microbiota after surgery.
Written by Chen Na and Fu Tanping
Pictures courtesy of the Department of Obstetrics and Gynecology
Edited by Xiao Xiong
