Technology advancements have enabled more treatment options for malignant lung nodules. Tapping into the well-equipped hybrid operating room at the National Infrastructure for Translational Medicine, the Department of Thoracic Surgery, PUMCH has recently combined intraoperative two-dimensional fluoroscopy (digital subtraction angiography, DSA) with electromagnetic navigation bronchoscopy-guided ablation for treating malignant lung nodules. This approach not only improves ablation precision but also reduces patient radiation exposure. The application of this clinical research has been supported by the National High Level Hospital Clinical Research Funding.
▲Thoracic Surgery and Anesthesiology teams were examining a patient's 3D reconstruction from images
According to the 2024 US NCCN Guidelines for Treatment of Cancer by Type: For single lesions, surgery remains the preferable choice if it’s tolerable; for multiple lung nodules, various local treatments such as surgery, ablation, and radiotherapy can be used.
Compared with traditional surgery, electromagnetic navigation bronchoscopy-guided lung nodule ablation is less invasive, tolerable for elderly patients and those with impaired lung function, and promises faster postoperative recovery. Compared with ablation through percutaneous puncture, this technique comes with a lower risk of complications like pneumothorax and bleeding, and can reach deep-seated lung lesions. Its main drawback is lower precision as respiratory motion causes lung nodule position to constantly change. According to literature, with electromagnetic navigation guidance alone, ablation accuracy is only about 60%. Combining it with intraoperative CT can increase accuracy to 90%-95%, but frequent scanning prolongs surgery and elevates radiation dose.
The commissioning of the hybrid operating room of the National Infrastructure for Translational Medicine brings hope for solving these challenges. Leveraging the hybrid operating room, the Department of Thoracic Surgery innovatively combined electromagnetic navigation bronchoscopy with intraoperative DSA, achieving precise guidance with lower radiation doses. Patients can get out of bed 2 hours after this minimally invasive surgery and be discharged after 1 day.

▲Thoracic surgeon Xu Yuan (right) and anesthesiologist Tang Bo (left) during surgery


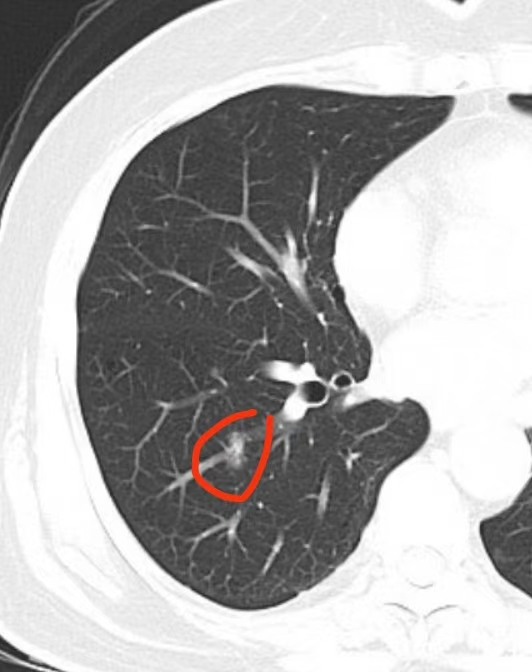
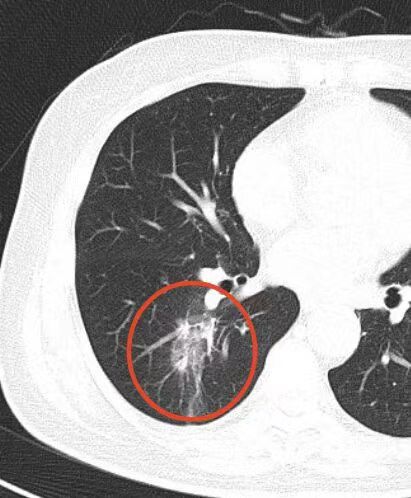
▲Comparison of two lung nodules before and after ablation: images on the left side are CT scans of malignant lung nodules; images on the right are CT scans on the first day after ablation, with ablation range covering the lesions
Dr. Li Danqing, Director of Thoracic Surgery, explains that this clinical approach offers effective local tumor control. It's particularly beneficial for patients who are not fit for surgery due to various factors, or in cases where surgery can't completely address all the lesions.
Written by Gan Dingzhu
Photographed by Sun Liang
Edited by Gan Dingzhu and Chen Xiao
Chief editor Duan Wenli
Supervised by Wu Peixin


