Recently, the team led by Professor Zheng Yuehong and Professor Chen Yuexin, Director and Deputy Director of the Department of Vascular Surgery, PUMCH respectively, published their clinical research findings on the endovascular treatment of vascular Behçet’s Disease (BD) in the “European Journal of Vascular and Endovascular Surgery” (a Q1 journal, or among the top 5%, as ranked by the Chinese Academy of Sciences). The study reported the team’s progress in endovascular repair of aortic pseudoaneurysms in vascular BD patients. It was supported by National High Level Hospital Clinical Research Funding.
BD, also known as the Silk Road disease, is a complex and rare chronic systemic vasculitis that often affects multiple organs in the body. Common clinical manifestations include oral and genital ulcers, and ocular inflammation. The prevalence of BD in China is approximately 14 cases per 100,000 people. Vascular BD is a specific type of BD characterized by vascular complications, with systemic vascular involvement for about one-third of the patients. Compared with other clinical phenotypes of BD, vascular BD progresses more rapidly and has a worse prognosis, especially when it affects large blood vessels and important branches. This leads to a significant increase in the incidence of postoperative severe complications and mortality, with the formation of pseudoaneurysms being particularly life-threatening.
Currently, the diagnosis and treatment of pseudoaneurysms in patients with vascular BD remain a global challenge, with limited systematically summarized experience available as reference to physicians. The affected blood vessels in vascular BD patients are fragile, which results in a higher risk of intraoperative rupture and bleeding. Surgeons must be highly skilled to perform on such patients. The vascular surgery team of PUMCH, in collaboration with other departments, has cumulatively diagnosed and treated over 100 vascular BD patients with pseudoaneurysms, one of the highest for international single-center reports, with aortic pseudoaneurysms accounting for the highest proportion.
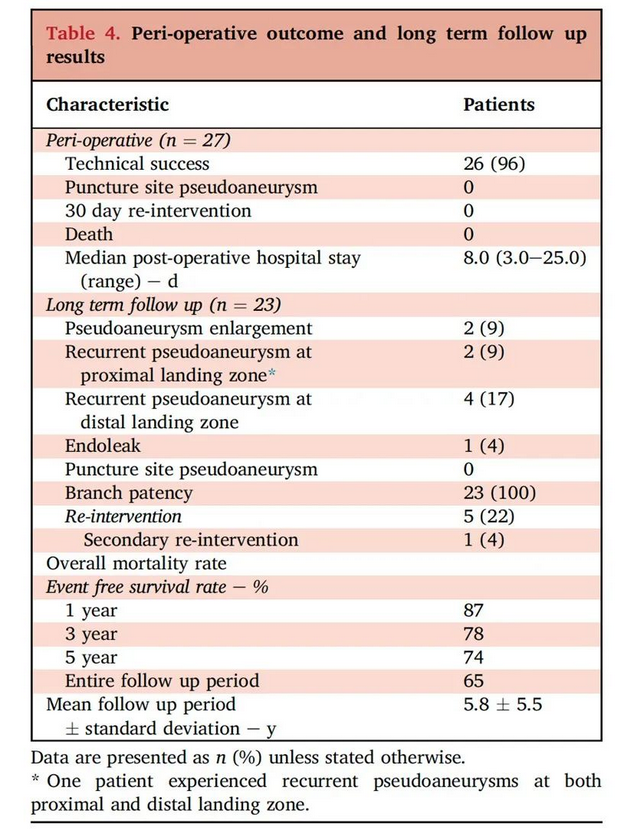
▲Perioperative and long-term follow-up results of vascular BD patients with aortic pseudoaneurysms
To find more compelling clinical evidence, the vascular surgery team conducted a retrospective analysis of vascular BD patients who underwent endovascular repair for aortic pseudoaneurysms. The study demonstrated a technical success rate of 96% in this patient cohort, with both perioperative re-intervention rate and mortality being 0. During the follow-up period, the branch vessel patency rate was 100%, and the incidence of puncture site pseudoaneurysms and mortality were both 0. Additionally, 73.9% of patients did not experience any significant adverse events, with 1-year, 3-year, and 5-year event-free survival rates being 87%, 78%, and 74% respectively. The overall outcomes of endovascular treatment were satisfactory, putting the team in an internationally leading position.
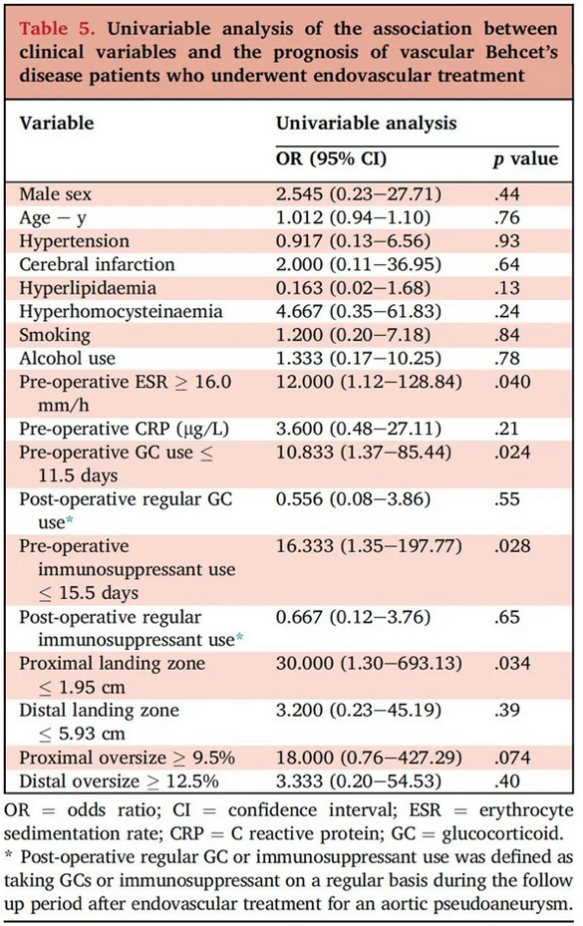
▲Univariate regression analysis was conducted to explore the prognostic risk factors for endovascular repair of aortic pseudoaneurysms in vascular BD patients
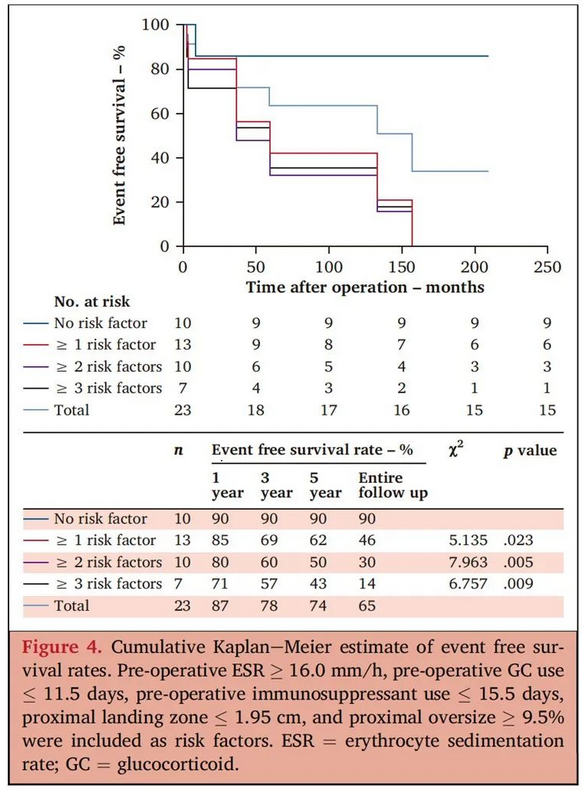
▲Risk stratification for predicting the long-term prognosis of patients after endovascular repair of aortic pseudoaneurysms in vascular BD
The research team revealed that by proactively controlling preoperative BD-induced inflammation, using glucocorticoids and immunosuppressants regularly and adequately, and selecting appropriate stents and landing zone, the efficacy and medium-to-long-term prognosis of endovascular interventions in patients with vascular BD can be improved. This study identified clinical monitoring indicators that provide a basis for improving the prognosis of vascular BD patients undergoing endovascular repair for aortic pseudoaneurysms and optimizing clinical decision-making by vascular surgeons.
This study, building on the know-how of the PUMCH vascular surgery team, further validates the reliability of endovascular repair in the clinical management of vascular BD patients with aortic pseudoaneurysms. It also, ahead of others, identified prognostic risk factors, providing a basis for improving medical care to patients with vascular BD. However, in the future, large-scale prospective multicenter clinical studies are still needed to establish more authoritative guidelines.
Written by Chen Xiao and Chen Yuexin
Edited by Xiao Xiong
Translated by Liu Haiyan
Reviewed by Cui Liqiang and Wang Yao
