Professor Chen Youxin and his team from PUMCH’s Department of Ophthalmology have published a significant paper in “QJM - An International Journal of Medicine” (JCR Quartile 1, IF: 13.3). This research focused on Purtscher-like retinopathy (PLR) in systemic lupus erythematosus (SLE), exploring its multimodal imaging features, systemic risk factors, and prognosis. This study, which compared PLR with the more common retinal microvasculopathy in SLE patients, is vital for improving fundus examination and evaluation of SLE patients.
PLR, a rare retinal vascular condition in systemic diseases including SLE, acute pancreatitis, pre-eclampsia, and renal failure, is characterized by sudden visual impairment, retinal edema, hemorrhage, extensive cotton-wool spots, and Purtscher flecken (clusters or confluent areas of whitish-gray lesions that appear around the optic nerve and posterior pole of the retina after widespread capillary network infarction). Its pathogenesis remains unclear. It is well recognized that retinopathy is strongly correlated with disease activity in SLE patients. However, limited studies has focused on PLR in SLE, including its potential risk factors and its comparison with common retinal microvasculopathy in SLE.
In this study, researchers conducted a retrospective analysis of 17 SLE patients (32 eyes) who were diagnosed with PLR from 2013 to 2022 following comprehensive ophthalmic examinations. For comparison, SLE patients diagnosed in the same timeframe but without retinopathy, as well as patients exhibiting retinal microvasculopathy (only manifesting cotton-wool spots, microaneurysms, hard exudates, and retinal hemorrhages, with better visual prognosis) were also included.
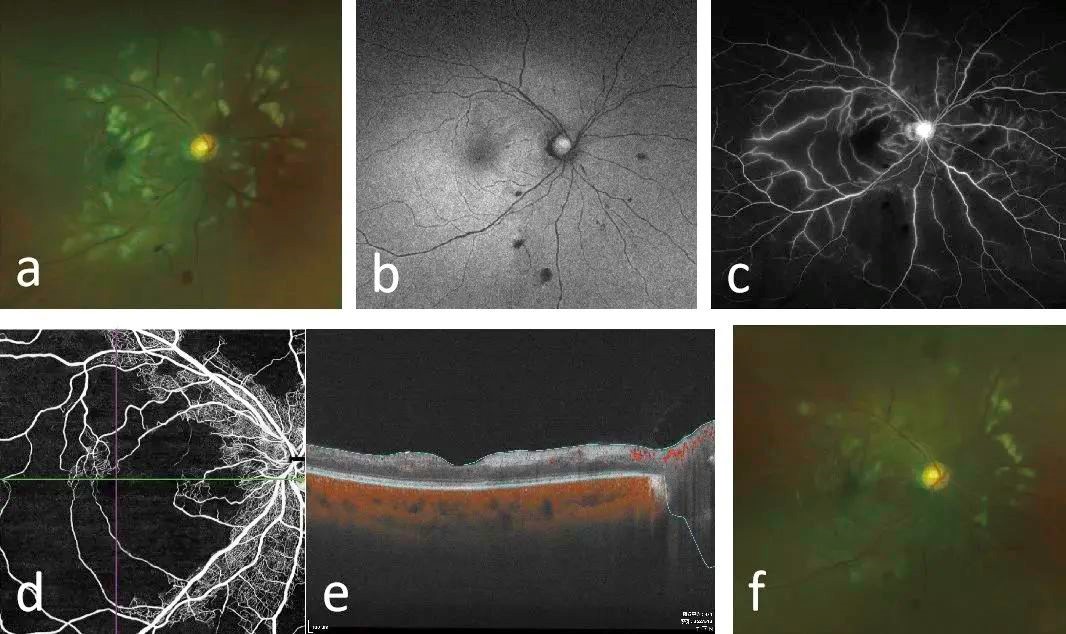
▲Multimodal fundus images (a-e) of an SLE patient with PLR, and lesion reduction after two months (f)
The study revealed that patients with PLR present with significantly younger age, higher proportion of hemolytic anemia, shorter SLE duration, higher SLE disease activity index-2000 (SLEDAI-2K) score, higher erythrocyte sedimentation rate (ESR) levels and lower hemoglobin (HGB) levels compared with SLE patients without retinopathy. Futhremore, the patients with PLR exhibited a significantly higher SLEDAI-2K score, higher ESR levels and increased white blood cell counts compared to those in the microvasculopathy group. During the follow-up period, 12 of the affected eyes underwent fundus laser or localized drug injections. In contrast, 14 affected eyes did not receive ophthalmic treatment. At the final follw-up, 84.62% of the affected eyes achieved condition stabilization, whereas 15.8% of affected eyes with PLR developed serious complications includingvitreous hemorrhage and retinal detachment or progression.
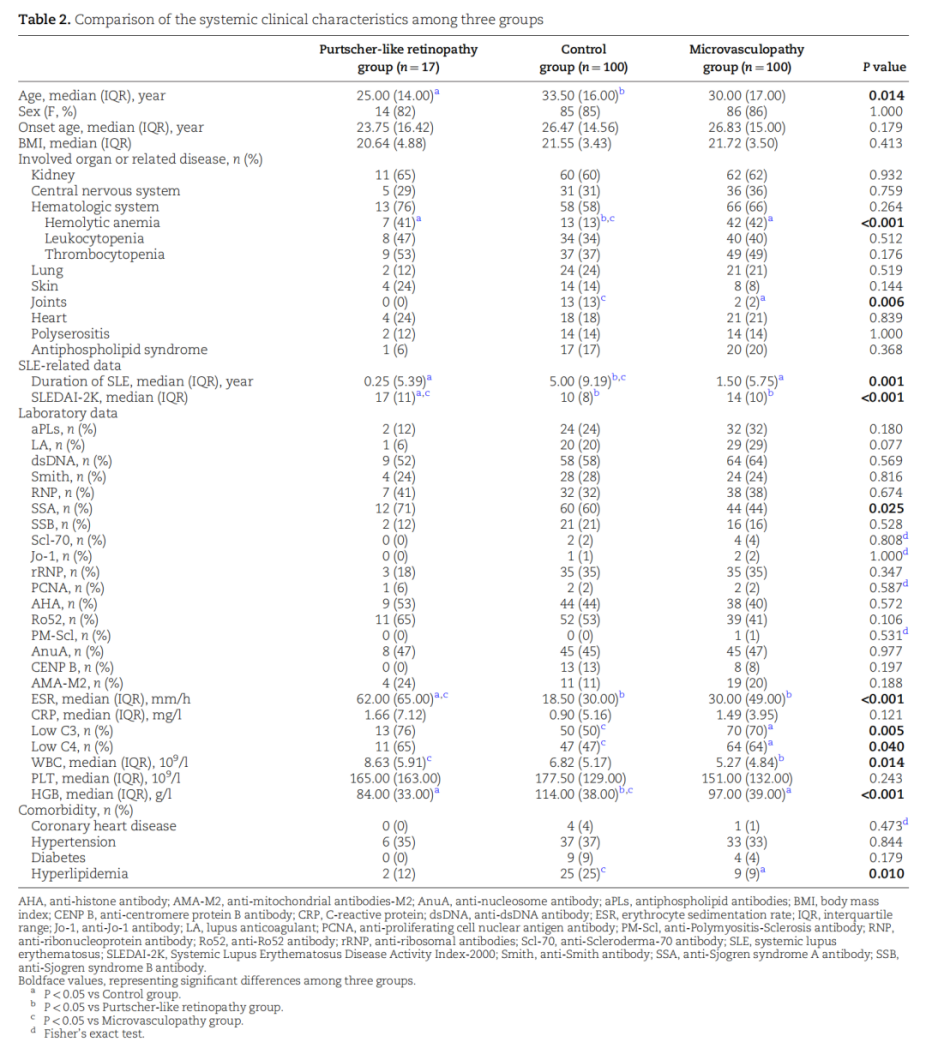
▲Comparison of clinical characteristics between the PLR group, the control group, and the microvasculopathy group
In summary, besides those with high disease activity, it is important for SLE patients, especially those who are younger, have a shorter disease duration, and su0w signs of hemolytic anemia, low HGB levels, and elevated ESR to undergo timely fundus examinations. early detection and intervention of PLR can significantly enhance the visual prognosis. In addition, given the distinct differences between PLR and common retinal microvasculopathy in SLE, particularly in clinical manifestations and systemic risk factors, further research is needed to elucidate the pathogenesis of PLR.
Link of the article: https://academic.oup.com/qjmed/advance-article-abstract/doi/10.1093/qjmed/hcad204/7259579?redirectedFrom=fulltext&login=false
Written by Meng Lihui and Wang Jingxia
Edited by Wang Jingxia and Chen Xiao
Translated by Liu Haiyan
Reviewed by Zhang Xia and Wang Yao
