The 51-year-old Ms. Zhu had a strange disease. Eight years ago, she suddenly started to have intermittent headaches and vertigo, which were diagnosed by the local doctor as hypertension. After she started to take antihypertensives regularly, her blood pressure began to fluctuate, sometimes high, and sometimes low. To make matters worse, her blood sugar also began to rise and was barely maintained with two insulin injections a day. Recently, she visited PUMCH, where her health was restored by a difficult operation, the 3D laparoscopic resection of paraganglioma in the retrohepatic inferior vena cava.
CT scanning revealed that Ms. Zhu had a tumor of approximately 47mm x 61mm growing in the posterior part of her pancreas head, which is a rare paraganglioma with an incidence of 1 in 100,000. It secreted a large amount of catecholamine that led to the symptoms besetting Ms. Zhu now. Once confirmed, the tumor should be surgically removed as soon as possible.
The tumor was buried deep in the abdominal cavity, making surgery difficult and the perioperative risk extremely high. The tumor was obscured by overlapping important organs such as the liver and pancreas in the front, with thick inferior vena cava running on its surface day and night, and tightly covered by portal vein and branches of abdominal aorta, which means adequate blood supply, and its boundary with surrounding tissues and organs was not clear. Moreover, the tumor secreted a large amount of hormones, which easily leads to drastic fluctuations of blood pressure and heart rate in the perioperative period.
During consultation with the specialized unit of PUMCH for intractable pheochromocytoma/paraganglioma diseases, the experts unanimously agreed that the Department of Endocrinology should first provide Ms. Zhu with systemic medications to regulate her heart rate, blood glucose and blood pressure and relieve the symptoms of headache and dizziness. After four months of medications, Ms. Zhu’s blood pressure and blood glucose stabilized, and the conditions were ripe for surgery.
The urology team quickly took over. They conducted a thorough preoperative preparation for Ms. Zhu, invited a multidisciplinary team for consultation, formulated a meticulous surgical plan, and performed a 3D visualized reconstruction of the paraganglioma.
On August 29, 2022, Dr. Wen Jin and Wang Wenda of the Department of Urology and Dr. Yang Xiaobo of the Department of Liver Surgery jointly performed the surgery on Ms. Zhu. The surgeons carefully dissected along the inferior vena cava proximally and used 3D laparoscopy to gradually turn the liver to expose the operative field. The inferior vena cava was seen to be elevated by the posterior tumor, and the lumen was significantly narrowed. The upper part of the tumor was deeply embedded into the surface of the liver, which made the surgical space narrow and the operation difficult. The blood supply around the tumor was rich, and there were multiple communicating vessels with the short hepatic vein and inferior vena cava.
Each step of the operation was like defusing a bomb. One surgeon was responsible for exposing the field of view while the other was responsible for peeling off the tumor, and the slightest tremor could cause the vessel to rupture, resulting in irreversible consequences. Finally, the urology team was able to completely peel off and remove the mass from the large interwoven web of blood vessels, organs, and tissues, with both kidneys intact. The anesthesiology department quickly followed up with norepinephrine and other medications, effectively preventing Ms. Zhu’s heart rate and blood pressure from fluctuating heavily. The Department of Intensive Care Unit gave Ms. Zhu a full range of postoperative supportive treatment. The smooth cooperation of the multidisciplinary team kept Ms. Zhu’s vital signs stable. She enjoyed a fast recovery.
Professor Wen Jin, Assistant Director of Urology, said: “Ms. Zhu suffered from a rare paraganglioma of the retrohepatic inferior vena cava. The tumor’s location was not ‘operation-friendly’, and the operation was a great test of the collaboration and resourcefulness of the operation team and the anesthesia management team. The success of it speaks to the comprehensive capabilities and techniques of PUMCH.”
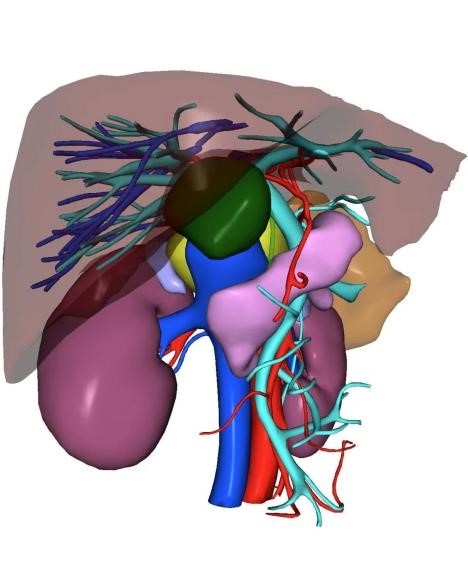
The patient’s paraganglioma was wrapped in layers of blood vessels and organs
Correspondent: Ma Xuan, Wei Mengchao and Wang Wenda
Reporter: Gan Dingzhu
Translator: Liu Haiyan
Editor: Fan Hua and Wang Yao
