When a large tumor was found in the “forbidden zone for surgery”, involving many important blood vessels in a patient having 30-year history of hypertension, which method will be the better solution: surgery or conservative treatment? Recently, Mr. He, nearly seventy years old had a huge mass in the caudate lobe of his liver removed thanks to the multidisciplinary team of PUMCH, which has given him a new lease of life.
In June 2022, Mr. He received a physical examination in PUMCH, which found a suspected hepatic space-occupying lesion. Further examination revealed a 9.3cm x 9.0cm mass in the caudate lobe of his liver, an indication of a high possibility of liver cancer. The feasibility of operation was the first and foremost issue in the repeated discussion between the Department of Liver Surgery (DLS) and Mr. He’s family.
With the cutting-edge combination systemic treatment protocol (e.g. TKI plus CIC), there was approximately a 10% probability of down-staging and conversion and a 30% probability of non-progression after treatment. Moreover, most of the patients experience the progression of liver cancer due to ineffective conservative treatment, in which case they would eventually lose the chance of operation. “We trust the capability of PUMCH. Please help us!” said Mr. He and his family, who made up their mind after thorough consideration.
How to maximize surgical safety is the second issue that the DLS had to solve. The Director of DLS, Prof. Sang Xinting, said that preoperative multidisciplinary consultation should be conducted to detail the surgical planning and develop various contingency alternative plans because “the safety of patients always comes first!”
The multidisciplinary team also went full steam ahead. Shen Le, executive deputy director of the Department of Anesthesiology, and Wang Huizhen, executive head nurse of the operating room, set up a team comprised of senior anesthesiologists and hepatology specialty nurses; the Department of Vascular Surgery was on standby with customized artificial blood vessels and a surgical coordination plan; the Department of Transfusion assured the supply of blood and pulled the blood refrigerator directly to the operating room for ready access; the ICU and hepatologists co-developed a postoperative monitoring treatment plan. Pan Jie, deputy director of the Department of Radiology performed hepatic artery embolization for Mr. He to reduce the risk of intraoperative bleeding by gaining insights into the main arterial blood supply source of the tumor.
After thorough preparation, the surgery was performed as scheduled by the surgical team made up by chief surgeons Mao Yilei and Du Shunda, and doctor Wan Xueshuai , etc.. After opening the abdominal cavity, a huge and appalling lump came into view. The upper end of the tumor had extended to the vena cava fossa and was compressing the root of the middle hepatic vein like a saddle. The hepatoduodenal ligament was pushed to the side by the tumor The three hepatic veins were squeezed and invaded.
The operators’ mind went through the plan that had been discussed preoperatively: the liver was completely dissected; the Porta Hepatis, both infra-hepatic and supra-hepatic inferior vena cava were controlled; the course of the right, middle, and left hepatic veins were identified with intraoperative ultrasound and marked on the surface of the liver; the tissues of segment IVa were dissected with ultrasound scalpel, CUSA, and bipolar electrocoagulation to fully expose the mass; the tumor was removed from the left hepatic vein, left and right hepatic pedicles, middle hepatic vein, and the right hepatic vein ... Each surgeon was fully concentrated and performed cautiously inch by inch. After a five-hour arduous battle, this extremely risky operation was successfully completed under the joint efforts. The patient’s vital signs remained stable, and the intraoperative bleeding was only 500ml. Upon realizing that the surgery went well and the tumor was completely resected, Mr. He’s family burst into tears. “Dad, we beat the odds!” his daughter said.
Although Mr. He was unaware of what had happened during the surgery, he could clearly recall the first morning after surgery. The clock was about to strike seven when he regained consciousness in ICU, and the first person he saw was Dr. Mao, who said in a gentle voice, “the most dangerous moment has passed. You can go back to the normal ward today.” Mr. He said, “I have no connection with the staff in PUMCH, but they took care of me like a family member. I am so lucky to have met such a good team so that having cancer even doesn’t mean total tragedy.”
While some people may regard high-risk surgery as “an intimidating journey”, Du Shunda believes that every cloud has a silver lining. “Sometimes, a family has nothing to count on but a doctor’s determination. Behind us is the unswerving solidarity and care of all departments of the hospital. We will definitely do our best because patients trust us with their lives.”
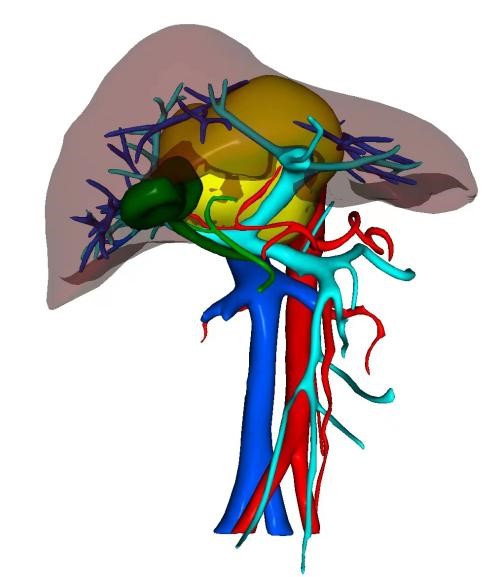
3D reconstructed image of the patient’s liver (yellow part is the tumor)

The patient sent a banner to express his gratitude to the surgical team. From left: Wan Xueshuai, Du Shunda, Mao Yilei.
Reporter: Gan Dingzhu
Correspondent: Wan Xueshuai
Picture courtesy: The Department of Liver Surgery
Translator: Liu Haiyan
Editor: Xu Haifeng and Wang Yao
