COVID-19 has emerged as a major global health threat since December, 2019. By April 1st, 2020, there were more than 800,000 patients with confirmed COVID-19 infection worldwide. Radiotherapy is continuous in treatment schedule. Interruption of the treatment or delay of the treatment may jeopardise therapeutic efficacy. Fuquan Zhang , Ke Hu and Hongnan Zhen from department of radiation oncology, PUMCH published a letter online on Radiotherapy and Oncology (official journal of the European Society of Radiotherapy and Oncology, IF 5.252), sharing PUMCH experience to relevant medical staff worldwide.
According to the clinical needs of the patients during the epidemic and the management experience of our department, we proposed a number of constructive suggestions:① Differential diagnosis: Acute radiotherapy pneumonia should be differentiated from COVID-19 pneumonia. According to the ‘‘Diagnosis and Treatment Protocol for COVID-19 (Trial Version 7)”, radiotherapy should be suspended or postponed among patients with fever. At the result of nucleic acid detection confirmed or suspected of COVID-19 infection, the patient will be transferred to the designated COVID-19 hospital for treatment. ② Make individualized radiotherapy plan:For patients with alternative therapy, radiotherapy is not recommended for the time being. Informing patients of the advantages and disadvantages of the radiotherapy, could help patients learn about the decision of the radio-oncologists. For patients indicated for adjuvant radiotherapy, postponing the start of radiotherapy until the epidemic is stable or even after the end of the epidemic is a reasonable choice. For patients indicated for neoadjuvant radiotherapy, appropriate extension of the course of oral chemotherapy can be an alternative approach. For individuals with emergent radiotherapy indications, radiotherapy should be intervened immediately. ③ Optimize the treatment mode:Treatment segmentation and dose could be adjusted by two or more experienced radio-oncologists. Stereotactic radiotherapy and shortening the course of treatment could also be considered based on evaluation of patient COVID-19 exposure risk. ④ Follow-up schedule:For patients with stable disease, the follow-up period should be more adjustable. For example, within the first two years after radiotherapy completion, the follow-up could be every 3–6 months. It is reasonable to postpone their next follow-up after the control of COVID-19 pandemic. ⑤ Diagnosis and treatment mode:With the help of tools like Wechat and network video phone, online multi-disciplinary treatment can be held to discuss the most optimal treatment plan for the patient, not only reduce the gathering but also decrease the possibility of COVID-19 infection. ⑥ Psychological counseling:Online health education and counseling could be performed regarding treatment principles, psychological counseling, nursing guidance and so on to lower the risk of anxiety and depression in cancer patients.
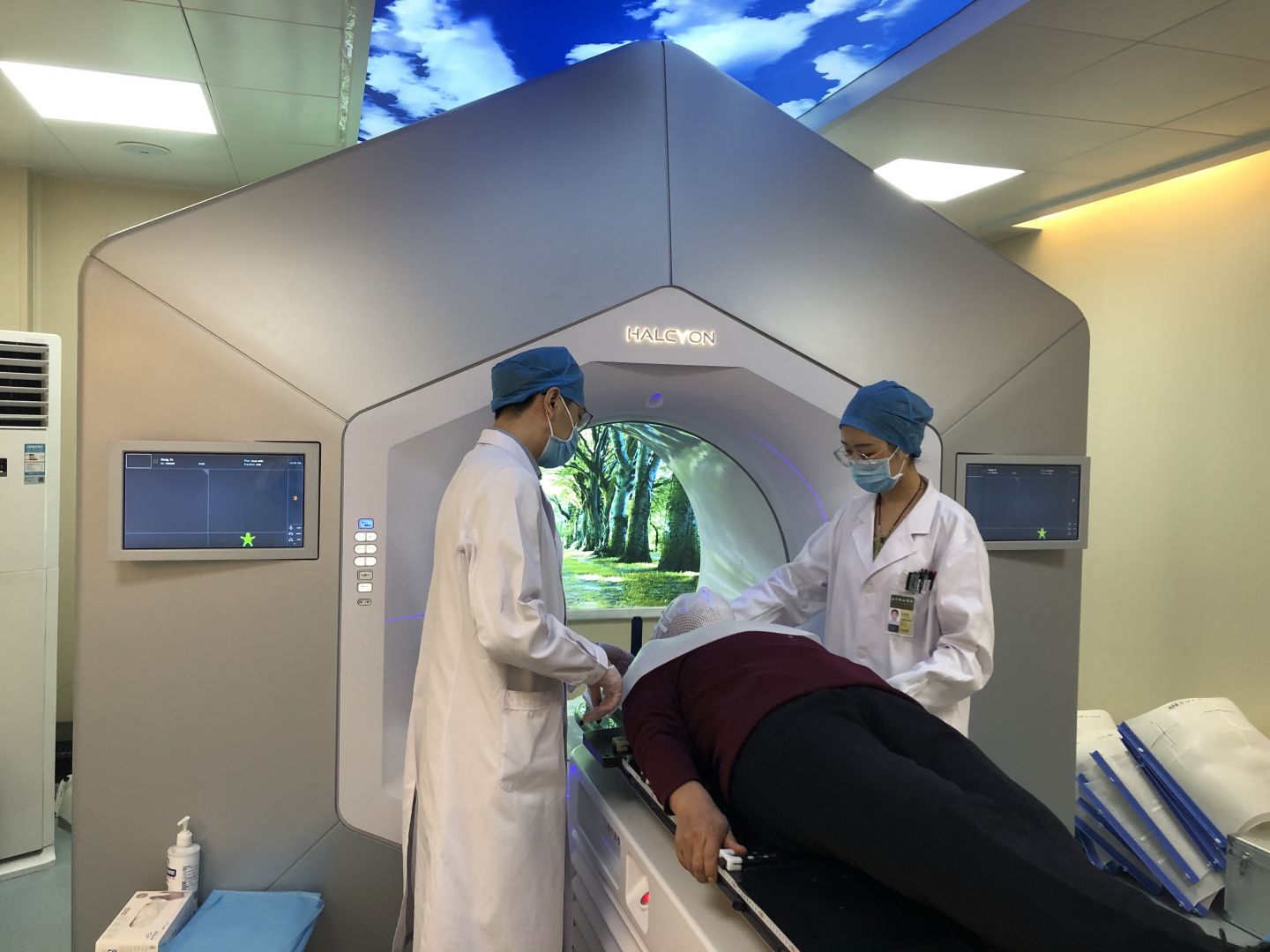
▲With proper protection, Department of radiation oncology, PUMCH guaranteed patient treatment during COVID-19 epidemic

▲Members of department of radiation oncology
Article Link: www.sciencedirect.com/science/article/pii/S0167814020302061
Writer: Hong-nan Zhen
Editor: Tan-ping Fu