Editor’s Note:
From May 22 to 26, 2023, a delegation consisting of four delegates from PUMCH and delegates from Peking Union Medical College (hereinafter referred to as the delegation) visited five institutions in the United States: NewYork-Presbyterian Hospital, Columbia University Vagelos College of Physicians and Surgeons, New York University Grossman School of Medicine, Westchester Medical Center, and the Rockefeller Archive Center. The purpose of this visit was to learn about the US experience and practices in curriculum reform and the transition from medical school to graduate medical education (GME), as well as to promote international collaboration. Let us examine the delegation’s activities and experiences more closely to stay up-to-date on medical education trends in the US.
In today’s world of mind-blowing innovation and transformation brought about by technologies like ChatGPT, AI and VR, how do we nurture medical students for the future? How do we set goals for cultivating talents and adapt the medical education model to the ever-changing information age? With these questions in mind, the delegation embarked on the 5-day US medical education tour, which was well-planned and packed with useful, meaningful activities thanks to the support and assistance of organizations like the China Medical Board (CMB).

▲The delegation at Columbia University Vagelos College of Physicians and Surgeons. Monica L. Lympson (fourth from left), Vice Dean for Education at Columbia University Vagelos College of Physicians & Surgeons; Barbara J. Stoll (sixth from left), Senior Advisor to CMB; Li Wenkai (seventh from left), CMB Chief Representative in Beijing
Through visits and in-depth discussions, we discovered that leading institutions in the United States, which are at the forefront of medical education innovation, have developed a set of theories suitable for efficient adult learning. These institutions fully leverage the empowering role of information technology to create models for personalized and precision medical education. In summary, these models have three main characteristics.
First, the medical education curriculum systems have been continuously optimized to cater to future needs. The Columbia University Vagelos College of Physicians and Surgeons has initiated the “Reimage” project, focusing on developing a curriculum system geared towards medical talent cultivation in 2050. NYU Grossman School of Medicine has boldly reformed its curriculum over the past decade, reducing the duration of medical school from 4 to 3 years and planning to fully implement the “C21” (Curriculum for the 21st Century) system based on the 3-year model. Through blending fundamental and clinical knowledge as well as interdisciplinary knowledge, among others, the teaching time for theoretical knowledge in medical schools across the United States has been reduced to 12-16 months. The “flipped classroom” approach has been widely applied, allocating more class time to case-based group learning and scenario-based simulation. This approach blends fundamental and clinical learning and motivates students to acquire knowledge and skills with greater initiative and efficiency.
We were most impressed by T2R (Transition to Residency), a course for the final year at NYU Grossman School of Medicine. Through the “Night on Call” simulation, this course improves the clinical skills of senior medical students. In addition, the design of distinctive courses such as Biomedical Informatics and Medical Decision SLIM (systems, leadership, integration, and management) speaks volumes about the forward-thinking nature of medical education.
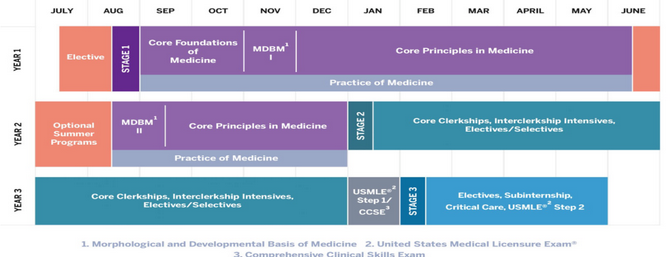
▲The Accelerated Three-Year MD Pathway of NYU Grossman School of Medicine (Source: official website of NYU Grossman School of Medicine)
Second, emphasis has been placed on the innovation of medical education concepts. NYU Grossman School of Medicine has proposed the new concept of precision medicine education and, to that end, has vigorously applied new technologies such as big data and artificial intelligence to medical education. In 2013, it established the Institute of Innovation in Medical Education. Currently, NYU Grossman School of Medicine has achieved customized medical student education, precision student assessment, and personalized training through multiple pathways, all based on big data analysis. The school has also developed Notesense, a natural-language-processing-based medical record analysis and feedback system for medical students and residents. Furthermore, 3D and VR has been leveraged in traditional anatomy courses to facilitate independent learning in anatomy.

▲Picture taken after the delegation interviewed Professor Robert I. Grossman (fifth from left)
Third, special attention has been paid to developing competent faculty. Both the Columbia University Vagelos College of Physicians and Surgeons and NYU Grossman School of Medicine suggested that the key to curriculum reform lay in educational leaders and course directors. To cope with the increasing workload of medical care and research, the affiliated hospitals of these two medical schools have both established a Coach system, allowing clinicians to take on some teaching work and offer long-term guidance to students. To physicians willing to shift to the teaching track, both hospitals put in place a clear pathway for promotion and steer attention, opportunities and resources in their favor when it comes to teaching training, post or position determination. This creates a favorable environment for physicians dedicated to teaching to thrive.

▲A VR-enabled class at NYU Grossman School of Medicine (Source: official website of NYU Grossman School of Medicine)
To advance medical education at PUMCH, the delegation proposed the following three recommendations. First, the hospital PUMCH and the medical school PUMC should seekcoordinated development, and establish a medical education research center. The clinical schools and departments of the hospital should take the lead in guiding medical education reform, designing talent training models that blend global and local perspectives, based on the medical talents in demand in clinical settings and the goals to be accomplished. Second, more investment needs to be made to increase IT adoption in medical education. Teaching materials and tools utilizing information technologies can improve students’ self-learning efficiency and enable personalization. Third, the medical curriculum should be re-evaluated with an eye toward innovation. Teaching methods could be modernized with information science. Assessment techniques should be made more goal-oriented. Faculty training should be enhanced so instructors can transform their roles and utilize IT for innovative teaching design.
Written by Li Yue, Pan Hui, Long Xiao and He Jing
Translated by Liu Haiyan
Reviewed by Li Yue and Wang Yao
