Recently, the latest review authored by Academician Zhao Yupei’s team from PUMCH was published in “Signal Transduction and Targeted Therapy” (IF: 38.104), which comprehensively covered the mechanisms of how metabolic dysfunctions in obesity and diabetes mellitus (DM) compromise anti-cancer immunity and fuel the initiation of pancreatic cancer, and provided novel insights into preventing obesity- and DM-related pancreatic cancer and future directions of relevant research.
Numerous clinical studies and high-quality meta-analyses have confirmed the carcinogenic impact of obesity and DM on the pancreas. Obesity and DM lead to alterations in hormone levels, microbiome dysbiosis, and metabolic remodeling, where the pernicious accumulation of substantial nutrients, metabolites, and other components provide precancerous and cancerous cells with mutagens, energy, hormones, and growth factors and support the interactions between the surrounding cells and cancer cells via autocrine/paracrine signals and rewired metabolism. These detrimental adaptations jointly create an inflammatory and immunosuppressive tumor microenvironment (TME) that eventually triggers cancer initiation owing to continuously strengthened pro-tumorigenic factors and compromised anticancer defense.
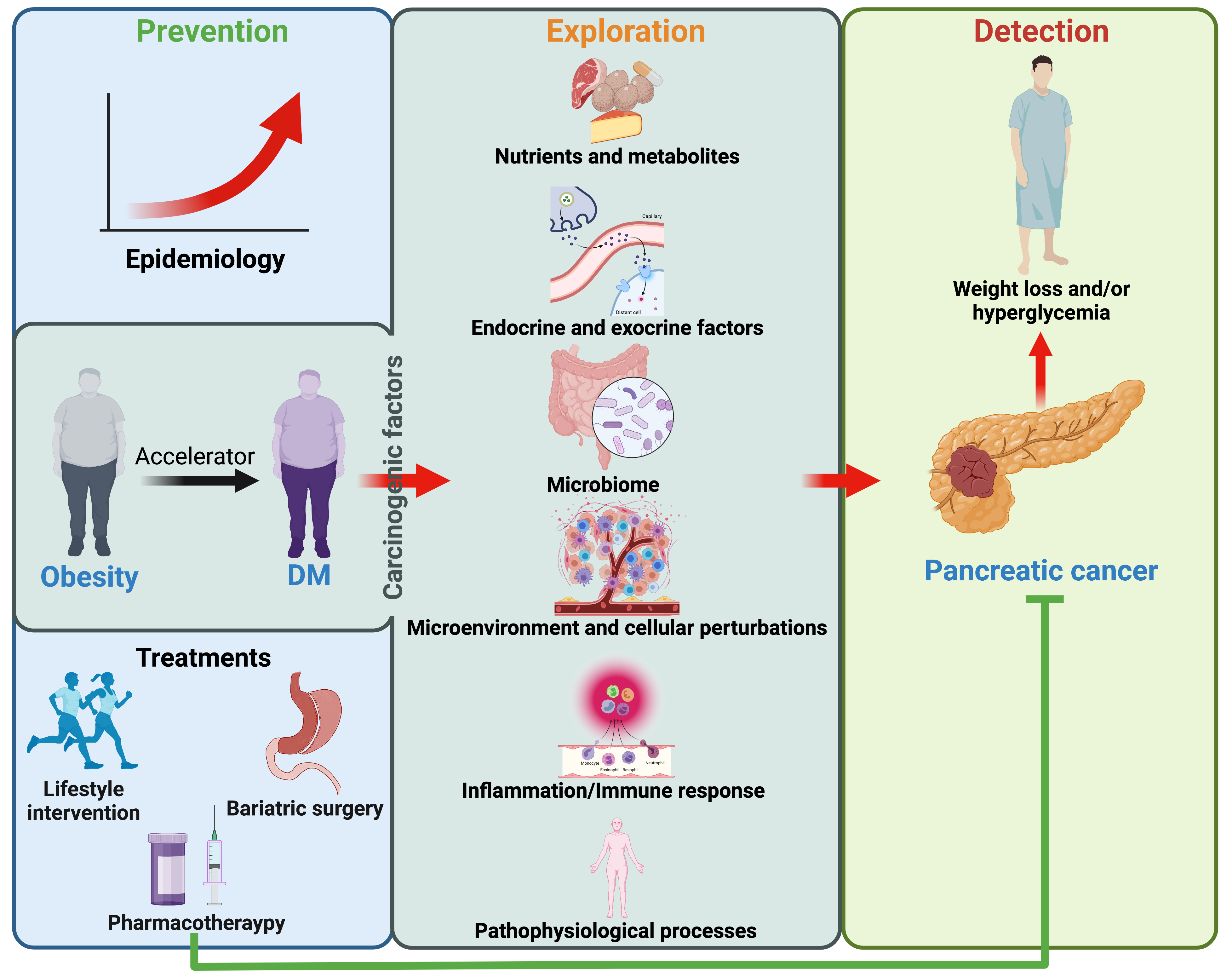
▲The intricate relationships among obesity, DM, and pancreatic carcinogenesis and the three most important values of relevant research.
Since the understanding of the associations between metabolic disorders and carcinogenesis is being deepened by recent findings, these results should serve the medical practices of pancreatic cancer from three dimensions:
First, the prevention of pancreatic cancer on the population level. Most treatments for obesity and DM can significantly reduce the risk of pancreatic cancer. Therefore, this risk can be preferably minimized by improving the efficacy of obesity and DM management.
Second, prevention of pancreatic cancer on the genomic level. A much clearer picture of the critical mutations that trigger pancreatic carcinogenesis and the subsequent genomic alterations has been demonstrated. Future efforts should be made to find the fuse of this “time bomb” set by obesity and DM or to cut off the fuse with the right “scissors”, which, hopefully, may help to reduce the occurrence of pancreatic cancer.
Third, early detection and timely treatment are critical to improving the overall outcomes of pancreatic cancer patients and are currently the most promising approach to making progress in clinical practice. The scientific community should take advantage of the emerging multi-omic analysis and advancing sequencing techniques to breed fruitful results in developing sensitive, feasible, reliable, and cost-effective biomarkers and early screening strategies for the population of obesity and DM by establishing modified disease models that highly replicate the original and natural pathogenesis through multidisciplinary cooperation and relentless innovation.
Written by Gan Dingzhu and Rexiati Ruze
Translated by Liu Haiyan
Edited by Hou Rui and Wang Yao
