On July 14, 2019, a 15-year-old girl with posterior mediastinal giant ganglioneuroma was admitted to the Department of Thoracic Surgery, Peking Union Medical College Hospital (PUMCH). A high-risk complex surgery was then successfully completed through multi-disciplinary collaboration.
Ganglioneuroma is a rare, benign tumor that grows slowly. It originates from sympathetic ganglion cells and mainly affects paraspinal, adrenal and retroperitoneal areas. Children and adolescents are more likely to be the victims. Surgical removal remains the mainstream treatment for this condition, and relapse rarely occurs after complete resection.
In this girl, the tumor was huge in size, adjacent to the spine, and closely related to the intervertebral foramen. A local hospital then referred her to PUMCH for thoracic surgery. Chest mediastinal contrast-enhanced MRI and PET/CT in our hospital revealed a dome-like soft-tissue mass sized about 10 cm next to the right thoracic spine, which was considered to be a ganglionoma after consultation with the Department of Pathology. After consultation with the Department of Endocrinology, oral administration of phenoxybenzamine tablets was scheduled for preoperative preparation.
During the rounds for complex surgeries inside the Department of Thoracic Surgery, the department chief Li Danqing recommended to initiate multi-disciplinary consultations before surgery due to the difficulty in surgical operation and the risk of intraoperative bleeding. One day before surgery, experts from the departments of thoracic surgery, orthopedics, neurosurgery, endocrinology, anesthesiology, and ICU participated in the discussion. The experts agreed that the lesion might be a ganglionoma without endocrine functions and an elective surgery could be arranged, during which the blood pressure and heart rate should be closely monitored. The surgery was expected to be extremely difficult and might cause massive trauma; therefore, the patient and her families should be adequately informed of the perioperative risks; if necessary, the patient could be transferred to the ICU after surgery. The 6th to 8th thoracic intervertebral foramen were suspected to be involved, and the possibility of cerebrospinal fluid fistula into the pleural cavity. Should be considered. The departments of orthopedics and neurosurgery might offer intraoperative consultations to assist with surgery. Liang Naixin's surgical team carried out detailed surgical planning and risk assessment before surgery, and decided to performed thoracoscopic exploration firstly.
On July 16, the patient underwent thoracoscopic exploration, adhesiolysis, and resection of posterior mediastinal mass. Intraoperative exploration revealed that the tumor was located in the posterior mediastinum, about 8 cm × 5 cm × 10 cm in size, with an envelope that was closely adhered to the chest wall and spine. After more than three hours of fine operation, the tumor was completely removed, along with its intact capsule. The departments of orthopedics and neurosurgery offered consultations during the surgery, confirming that no vital structures such as dura mater and nerve root were not damaged and no extended tumor resection was performed. With the careful control of the anesthesiologist and the close cooperation of the nurses in the operating room nurses, the patient's condition was stable. On the fourth postoperative day, the patient recovered well and was discharged.
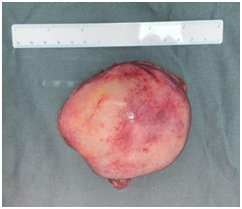
(Photo courtesy of the Department of Thoracic Surgery)
